Health officials and news headlines have announced that it has never been more important to get this year’s flu vaccine. The worry is that trying to accommodate influenza sufferers will snap health systems that are already seriously overstretched by COVID-19 patients. The 2021 northern hemisphere seasonal flu vaccine is now available, and many people are taking this warning seriously, wanting to do their part by staying healthy and preventing flu infections that could land them or others in hospital.
Good intentions aside, how realistic are expectations that the flu vaccine will reduce hospitalizations? Is there a good argument for individuals to get vaccinated? That is hard to say with certainty, but there are many factors to consider, including:
- Vaccine effectiveness
- Disease transmissibility, severity, and prevalence
- Vaccine risk
Vaccine effectiveness
BIG Media contributor Lee Hunt, in Understanding vaccine effectiveness and breakthrough, quotes the definition of vaccine effectiveness (VE) as “the percentage reduction in the incidence of disease among vaccinated persons compared with unvaccinated persons.” For example, in an unvaccinated group, 100 people might become infected with a virus. If, in a similar sized vaccinated group, only 10 get infected, the VE is (100-10)/100, or 90% effective.
Let’s look back at some historical flu numbers for context. In the United States, from 2004 to the present, the effectiveness of annual flu vaccines has varied from -52% to 70%.[1] Nationwide adjusted median annual values are shown in Figure 1 with the minimum and maximum range for each year overlain for context. A negative vaccine effectiveness means that, alarmingly, vaccinated people have a higher likelihood of contracting the flu than non-vaccinated people.
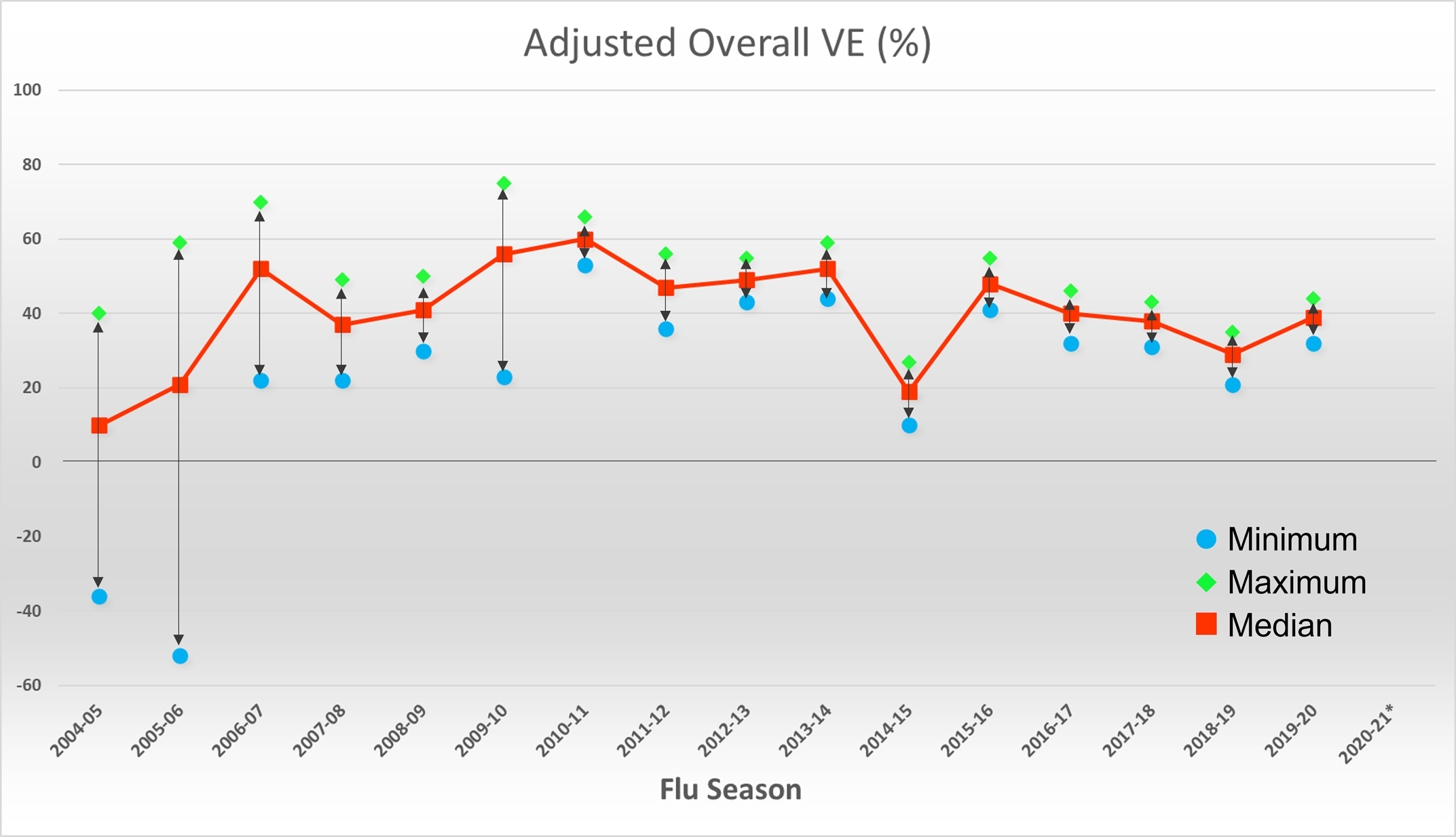
Figure 1: Flu vaccine effectiveness, U.S., 2004-2021. *Note that 2020-21 did not have enough data to determine flu vaccine effectiveness.
Disease transmissibility, severity, and prevalence
Transmissibility of a virus is measured as its “reproductive rate”, or “R” value, described in more detail in the BIG Media article Examining the effectiveness of restrictions and the path to COVID eradication. R0, the pristine reproductive rate, is the number of secondary infections that are generated from an initial case prior to any element of the population becoming immune and prior to any mitigation strategies. A higher R value means the virus spreads faster.
Typical median values of R0 for the flu range from 1.28 (seasonal flu) to 1.65 (pandemic flu).[2] These numbers can vary widely and have considerable uncertainty. The 1918 Spanish flu R-value estimates ranged from 1.47 to 2.27, with a median of 1.80.
Disease severity is measured based on intensity thresholds and is categorized as low, medium, or high.[3] The table below shows the severity category for recent flu seasons by age group.
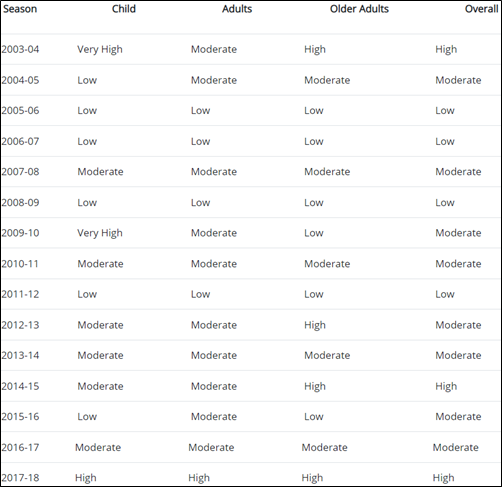
Table 1: Flu severity assignment in the U.S., by season and age group. Source: How CDC Classifies Flu Severity
Prevalence is about whether or not there is a flu virus to catch. In another BIG Media article, Where did the flu go – and do we miss it?, we point out the drastic reduction in flu infections in 2020 (Figure 2). The reasons for this reduction are discussed in more detail in the article, but the point is that we still seem to be missing the flu. Figure 3 shows this chart updated to show October 2019 to October 2021.[4]
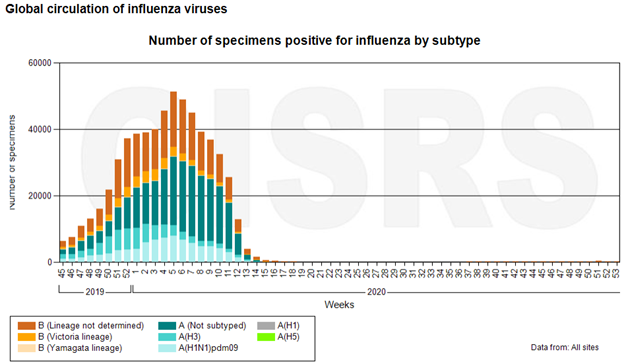
Figure 2: Global flu incidence by type and week, to the end of 2020.
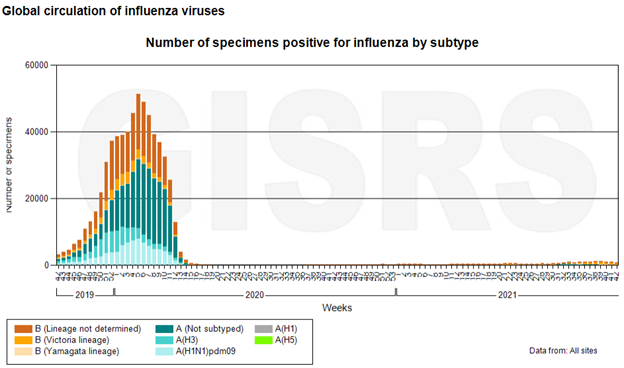
Figure 3: Global flu incidence by type and week, from October 2019 to October 2021.
You may have noticed that in the chart in Figure 1, the 2020-21 flu season has no value for the vaccine effectiveness. This is because there was simply not enough data to determine a statistically reliable number. This persistent lack of flu incidence is important in a discussion of vaccines because, every year, a World Health Organization (WHO) technical committee meets to determine the strains that will be included in that year’s vaccine.[5] If there is no flu to speak of, it is difficult to determine what strains to include. In years in which the flu strains in the vaccine do not match the actual strains in circulation during flu season, vaccine effectiveness is very low.
Vaccine risk
If there is a low chance of catching the flu, and if the vaccine effectiveness is potentially quite low because of lack of data to guide the composition, the risk of side effects from the vaccine itself becomes a more significant consideration. A 2012 report investigated all documented adverse effects of many vaccines, including the flu.[6] Table 2 shows the findings for 26 separate conditions that have been linked to the flu vaccine to some degree. The conclusions indicate inadequate evidence to either support or reject the links in 22 of these conditions. In only two conditions, the report favours rejection of the links (Bell’s palsy, and asthma exacerbation or reactive airway disease). The report favours acceptance in one – oculorespiratory syndrome – and convincingly supports the anaphylaxis connection.
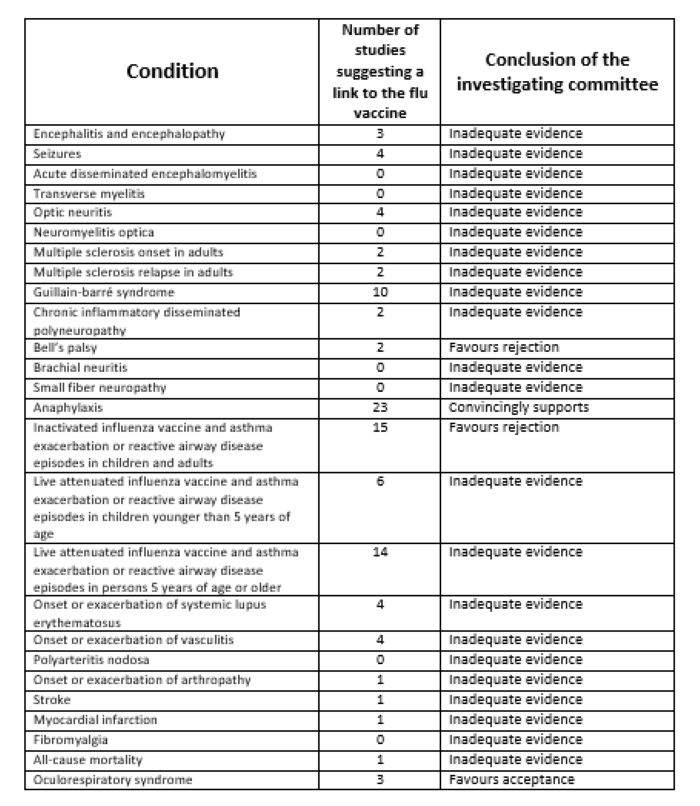
Table 2: Investigation results for medical conditions that were linked to flu vaccines.
Now, what about the main reason cited for getting the flu vaccine this year – that of reducing the burden on the health care system by reducing hospitalization resulting from the flu? A 2014 Alberta government model of anticipated future hospitalization relative to the proportion of the population vaccinated was shown in the BIG Media article COVID-19 is definitely not the flu(Figure 4). The reasonable expectation was that with increasing vaccination rates, hospitalization rates would decrease, eventually to almost zero.
However, the actual results did not play out as projected. As shown in Figure 5, hospitalization rates did not decrease as expected, but in fact increased – in some years, quite significantly.
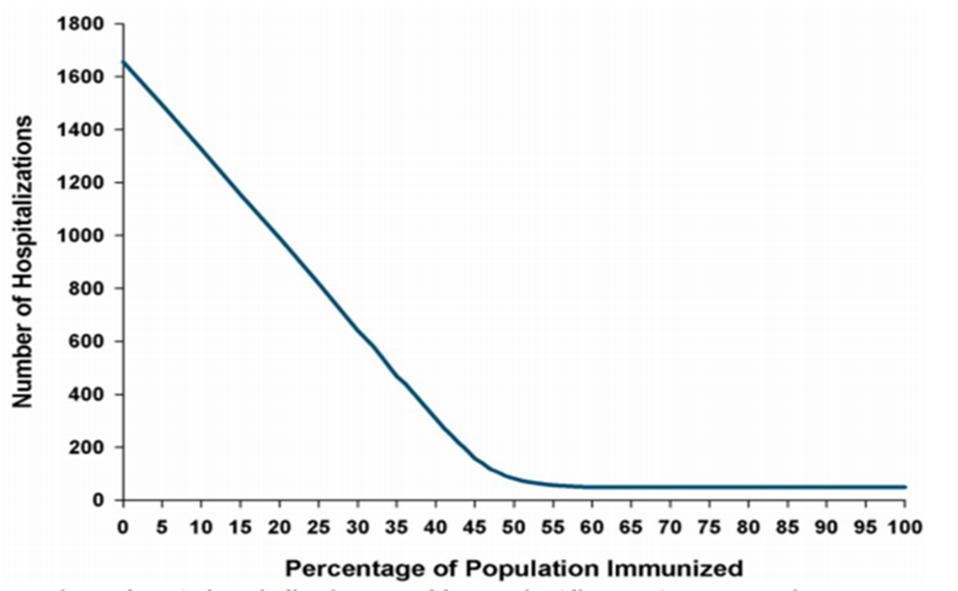
Figure 4: Projected hospitalizations as a function of the percentage of the population immunized.
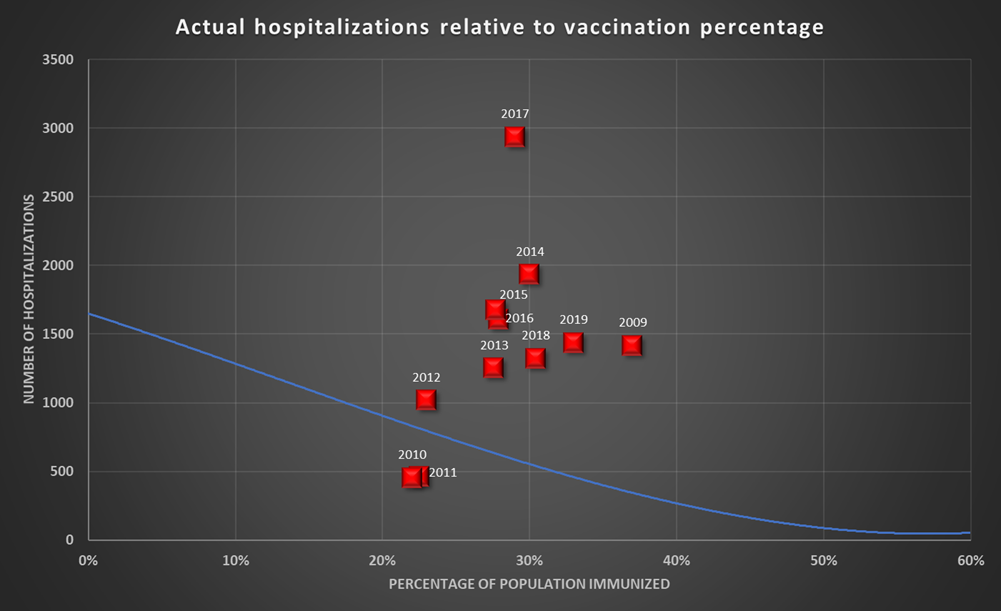
Figure 5: Actual hospitalizations relative to vaccination percentage, Alberta, Canada. The blue line represents the modeled forecasts at the appropriate scale.
In any case, with the low incidence of flu around the world since March of 2020, hospitalizations and deaths attributed to flu have correspondingly plummeted. Flu infections have begun to increase globally from the low in the same period in 2020, but they are still well below 2019 (Figure 6).[7] Incidentally, in Alberta, there were zero lab-confirmed cases in the 2020-21 flu season. In the 2021-22 season so far, there have been six cases, with no hospitalizations and no deaths.
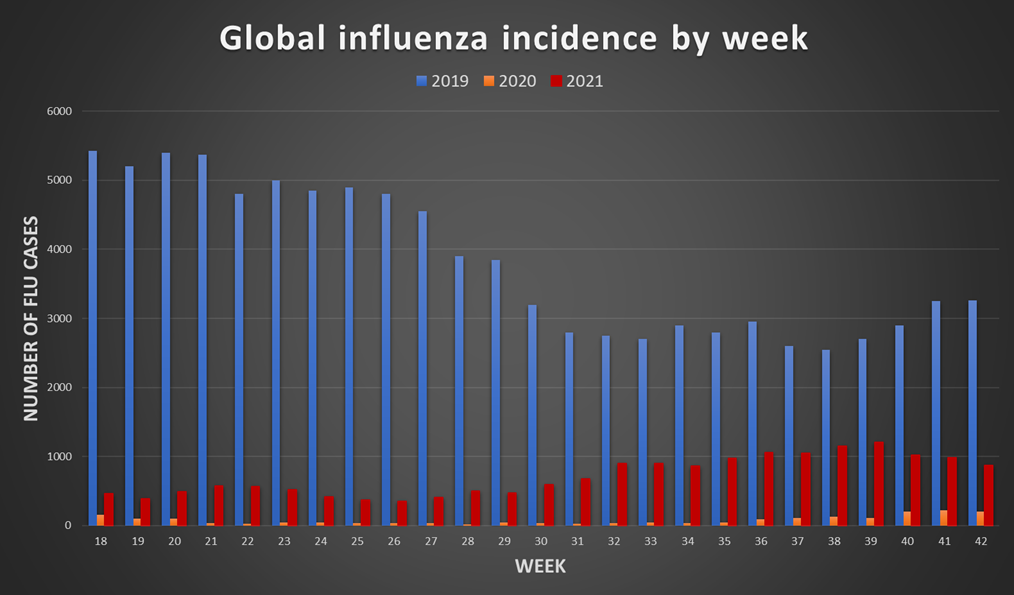
Figure 6: Global influenza cases from week 18 (May 3) to week 42 (October 17), for 2019 (blue), 2020 (orange), and 2021 (red). Source: WHO FluNet
While the arguments for the flu shot this year are not particularly compelling, we should avoid using these arguments to support a polarizing black or white position: vaccines work, or vaccines don’t work. It is always a matter of weighing the benefits and the perceived consequences in the context of the data.
We should also resist becoming complacent about disease. Just because we cannot see the threat, does not mean it is not there, waiting for us to let down our guard. In the absence of the greater evil (the disease), the lesser evil (prevention or mitigation) looms large – from a data perspective, a metaphorical scale change.
However, this year at least, indications point to a small threat from the flu, and an even smaller justification for vaccination. In this context, therefore, it becomes more a decision of individual conviction or vulnerability (age or compromising medical condition) than one of public health.
[1] Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases, Seasonal flu vaccine effectiveness studies, accessed October 26, 2021.
[2] Biggerstaff, M., Cauchemez, S., Reed, C. et al. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infect Dis 14, 480 (2014).
[3] How CDC Classifies Flu Severity, accessed October 31, 2021.
[4] https://apps.who.int/flumart/Default?ReportNo=10 accessed October 31, 2021.
[5] Recommended composition of influenza virus vaccines for use in the 2021-2022 northern hemisphere influenza season
[6] Kathleen Stratton, Andrew Ford, Erin Rusch, and Ellen Wright Clayton, Editors; IOM (Institute of Medicine). 2012. Adverse effects of vaccines: Evidence and causality. Washington, DC: The National Academies Press. Institute of Medicine, ISBN 978-0-309-21435-3, p293-421,
[7] Global Influenza Programme
(Laurie Weston – BIG Media Ltd., 2021)


Another important factor I have heard discussed that might need clarification is that ‘if we haven’t been sick with anything in 20months, we will be more likely to experience more severe symptoms resulting from the flu because our immune systems are out of practice’.
Otherwise, from what i can tell, predicting severity is uncertain so perhaps this is one of those decisions where being consistent might make the difference.
I have seen similar comments, but since it’s not certain what strains will emerge this year, it’s hard to say how prepared we will be either with a vaccine, or natural immunity from previous exposure. This is far from an exact science, Christa. When I was researching this article, that was the common theme in most of what I read.