While we were distracted by COVID-19, a strange thing happened: the flu disappeared. Just take a look at the striking chart below from the World Health Organization (WHO) showing global flu cases plummeting from normal levels in February 2020 to almost nothing by May 2020, and staying there for the rest of the year.[1]
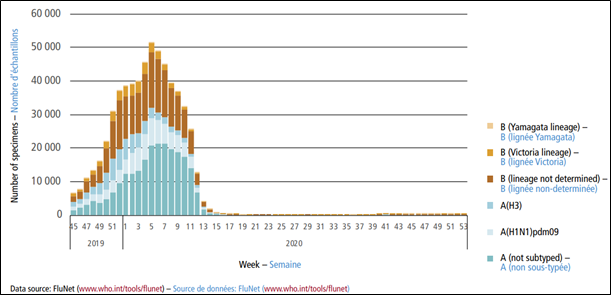
Chart 1: Number of global influenza detections by subtype between November 2019 and December 2020. Source: WHO.
Flu season has been an unpleasant part of winter for as long as we have had winter. So, why did it quietly fade away in 2020? As we documented in a recent article, COVID-19 is definitely not the flu. Will the flu be back?
It is likely no coincidence that flu infection rates decreased sharply with the community mitigation and hygiene guidelines promoted or imposed by governments around the world in response to the COVID pandemic. The deliberate interruption in typical social activity also interrupted influenza transmission.
A similar pattern was observed in Hong Kong during the 2003 SARS (SARS-CoV) outbreak.[2] The first confirmed SARS case was documented there on March 11, 2003, and the last one, June 2, 2003. This period of aggressive social curtailment and hygiene campaigns overlapped the typical flu season in Hong Kong (March to September). As Chart 2 shows, the incidence of respiratory virus infections while SARS was active was considerably lower than the average of the corresponding months in the reference period (1998-2002).
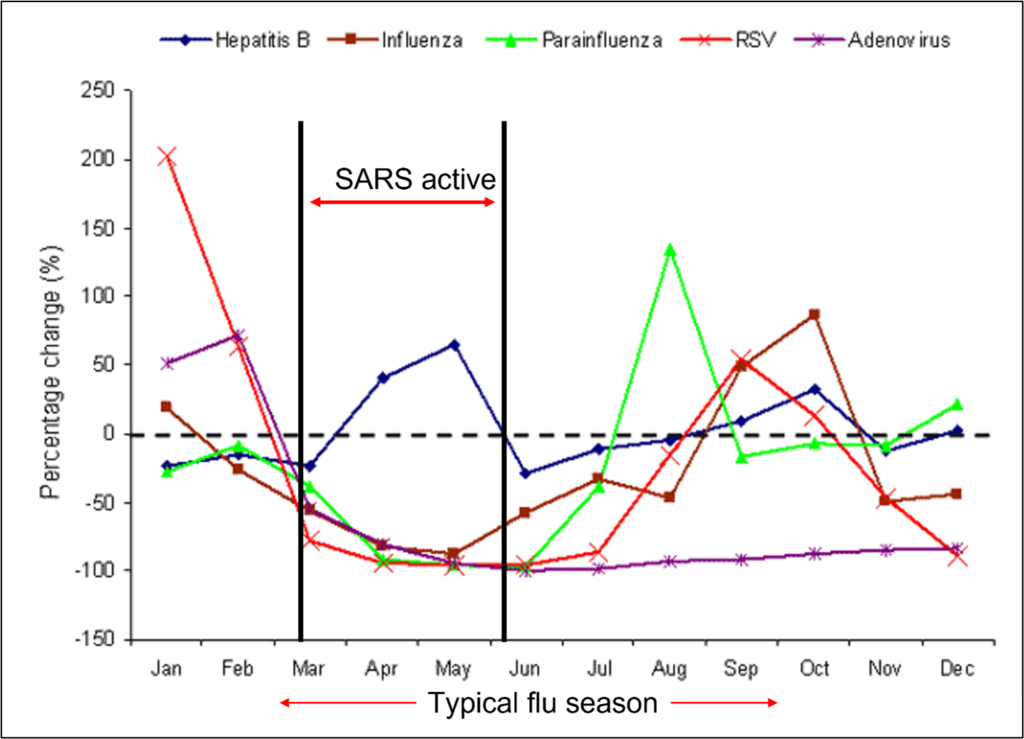
Chart 2: Change in proportion of positive specimens in Hong Kong in 2003 for various viruses with reference to period 1998–2002.
In addition to the relatively obvious effects of intervention, however, the WHO report mentions a phenomenon called “viral interference” that implies viruses attacking viruses. The theory goes that viral pathogens not only interact with the host cells, but interact with each other within the host. Therefore, virus-to-virus interactions can affect the success of one while inhibiting the other (in the case of two viruses fighting it out). As SARS-CoV-2 (COVID-19) and types of influenza are all respiratory viruses, they are in competition for the same cells. Consequently, COVID-19 can inhibit the flu virus. But the opposite can also happen; people who test positive for flu are less likely to test positive for COVID.
An associated effect called “cross-protection” involves a previous or incumbent virus “priming” the immune system to be more effective against a different but related virus. This means that people who have recently had flu or another type of respiratory virus and are then exposed to COVID potentially have greater natural protection. This effect has been observed in flu/common cold competition,[3] and between flu and other respiratory viruses such as Respiratory Syncytial Virus (RSV).[4]
On the microscopic level, there is an epic struggle going on between and amongst viruses, and our immune cells. It is interesting to imagine that perhaps an orchestrated alliance between the immune system and the more benign of the viruses might increase our defences against a more sinister one like COVID-19; a partnership with the lesser of two evils, so to speak. Maybe trying to prevent flu infections increases our vulnerability to more severe viruses.
We know as a society that severe social restrictions must be a temporary measure, so while those are shown to be effective, they are unsustainable. Vaccine development is an important component of pandemic preparedness, but effective vaccines lag the onset of a new virus. Strengthening our immune systems with improved overall health and, yes, exposure to viruses are natural and vital mechanisms of protection.
Will the flu come back? Yes, most likely, as is the case in Chart 2 after the SARS 2003 outbreak was over and people started to mingle again, sharing germs. In the interest of our long-term health, I kind of hope so.
[1]Erik A Karlsson, Piers Andrew Nicholas Mook, Katelijn Vandemaele, Julia Fitzner, Aspen Hammond, Vanessa Cozza, Wenqing Zhang, Ann Moen, Review of global influenza circulation, late 2019 to 2020, and the impact of the COVID-19 pandemic on influenza circulation, World Health Organization WEEKLY EPIDEMIOLOGICAL RECORD, NO 25, 25 JUNE 2021, p241-264.
[2] Lo J, Tsang T, Leung Y, Yeung E, Wu T, Lim W. Respiratory Infections during SARS Outbreak, Hong Kong, 2003. Emerg Infect Dis. 2005;11(11):1738-1741.
[3] Sema Nickbakhsh, Colette Mair, Louise Matthews, Richard Reeve, Paul C. D. Johnson, Fiona Thorburn, Beatrix von Wissmann, Arlene Reynolds, James McMenamin, Rory N. Gunson, and Pablo R. Murcia, Virus–virus interactions impact the population dynamics of influenza and the common cold, PNAS, December 26, 2019, vol. 116, no. 52, 27142–27150, accessed August 15, 2021.
[4] Waterlow NR, Flasche S, Minter A, Eggo RM. Competition between RSV and influenza: Limits of modelling inference from surveillance data. Epidemics. 2021 Jun; 35:100460. doi: 10.1016/j.epidem.2021.100460. Epub 2021 Mar 26. PMID: 33838587; PMCID: PMC8193815.
(Laurie Weston – BIG Media Ltd., 2021)


(Apologies, I hit the wrong button)
Meant to finish with, Is it all just viral competition? How does this compare to multiple strands of flu in our flu season? Thx
Hello, interesting article. I noticed no mention of the PCR test being unable to truly identify Covid-19 from other similar flu viruses (this came from the developer of the PCR test)? So does false-positives play a role? I ask because if people could contract Covid-19, then surely they could contract the regular flu..? They transmit in similar ways so why one and not the other?
Thx