In previous BIG Media articles (Assessing the relative lethality of COVID-19: a Canadian case study, COVID clarification – a tale of two tales), we compared COVID-attributed deaths to other causes of death of all types to provide context for the impact of COVID-19 in its first year. This was enlightening in many ways, but diseases such as cancer and heart disease are not contagious, and deaths from these causes are therefore unlikely to spread or suddenly increase exponentially. Viruses on the other hand, if unchecked, have the potential to go, like the latest cool online video, umm, viral.
There have been claims by skeptics on social and other media that COVID-19 is “just the flu” and as such is not worthy of the aggressive global response witnessed to date. This article will address the first part of that assertion, which will perhaps provide perspective for the second.
How do COVID deaths relate to flu deaths?
Our dataset for this investigation is from Alberta, Canada, and represents all deaths of all causes from 2001 through 2019.[1] Focusing on this province with a population of about 4.44 million provides the benefit of consistency in data reporting and compilation. Causes of death other than COVID have not yet been made available by the Alberta government for 2020. However, preliminary flu data for the 2020/21 flu season (September to April) shows zero confirmed cases in Alberta.[2] There have likely been unreported cases; nevertheless, there were no hospitalizations, no intensive care (ICU) treatments required, and no flu deaths.
Taking a broader view over the last 19 years and focusing only on deaths caused by viruses (Chart 1, left) and by influenza specifically (Chart 1, right), we see that the average of all virus deaths is 115 per year and, of flu alone, approximately 45 per year. The data in both charts is for all ages and genders and has been normalized to the 2020 population.
Comparing the 2,022 COVID deaths in 2020 (March 2020 to March 2021) to 69 flu deaths in 2019 and the 19-year average of 45, leads us to the conclusion that COVID has been convincingly more deadly than all viruses or influenza alone in recent history. This contrast in deaths is our first clue that COVID-19 is not the flu.
Chart 1: Total deaths from all viruses, including influenza, viral meningitis, viral hepatitis, and other unspecified viruses, compared with deaths from COVID-19 (left); total deaths from influenza only, compared with deaths from COVID-19 (right).
Of course, as with all data-driven investigations, we need to look deeper to understand the whole story. We will start with a little background on viruses, influenza, and pandemics.
Infectious diseases are a host’s response to unwelcome foreign pathogens such as viruses, bacteria, fungi, and parasites invading our bodies. Fungi (yeasts, molds) and parasites (worms, lice, ticks) are organisms that are quite easily – though not pleasantly – imagined in the minds of the general public. Viruses and bacteria, however, are less understood. The comparison shown in Chart 2 should help clarify the differences between the two tiniest pathogens.
Antibiotics and other treatments have been extremely successful at curing infections due to bacteria, fungi, and parasites. Although there has been progress in antiviral development (particularly for Hepatitis C),[3] there is no effective cure for diseases caused by viruses – only treatment of symptoms.[4] Hence the focus on prevention by good overall health, behaviour (education, hand washing, isolation when sick, etc.) and immunization.
Chart 2: Virus versus bacteria comparison
Our second clue that COVID-19 is not the flu is that they are caused by different viruses.
Influenza, or the flu, is caused by the Influenza Type A, B, C, or D virus. Influenza A and B are the most common in humans. Type A can have an animal (zoonotic) origin, such as birds, pigs, horses, and other warm-blooded creatures,[5] but Type B is only known in humans and seals.[6] Influenza A and B are the causes of the “seasonal flu” for which a specific vaccine is developed every year based on the subtypes, or strains, of each type that are active that particular year.[7] (More about the flu vaccine later.)
COVID-19 is the disease caused by novel coronavirus SARS-CoV-2. There are seven known coronaviruses, which can also have zoonotic origins such as bats, mice, and dromedary camels.[8] Four of these types cause mild common cold symptoms, and three (the novel ones) can cause more serious lower respiratory diseases.[9]
A pandemic is defined by the World Health Organization (WHO) as “a worldwide spread of a new disease … [for which] most people do not have immunity.”[10] All previous viral pandemics declared, or known of, in recorded history have been caused by Influenza A. The COVID-19 pandemic is the first time a coronavirus has been responsible.[11] Interestingly, AIDS, which is caused by the HIV virus and has killed about 35 million people since it was identified in 1981,[12] is termed a “global epidemic” by the WHO, not a pandemic.
H1N1 pandemic
Prior to 2020, the most recent pandemic declaration was in 2009, in response to the Influenza A/H1N1 virus (swine flu). According to a WHO Bulletin report, however, the declaration of the 2009 H1N1 pandemic has been questioned by many regarding the merit of the pandemic designation.[13] H1N1 turned out to be not nearly as widespread nor as deadly as the WHO’s own criteria stipulated. The report alludes to improper influence related to ties between WHO H1N1 advisers and corporate interests.
In fact, we can see in Chart 3, showing only the Influenza numbers, that total deaths in Alberta in “pandemic” year 2009 due to flu (shown in the blue bar) were not outside of the recent ordinary spectrum. Different sources within the Alberta government report flu deaths in 2009 ranging from 30 to 82, illustrated by the additions of the green and orange extensions to the 2009 data point.[14] There is always uncertainty in data. Often, uncertainty is not reported in media articles, however subjectivity and judgement are inherent in nearly every data story, particularly one that involves a decision in a potentially ambiguous situation, such as a definitive single cause of death.
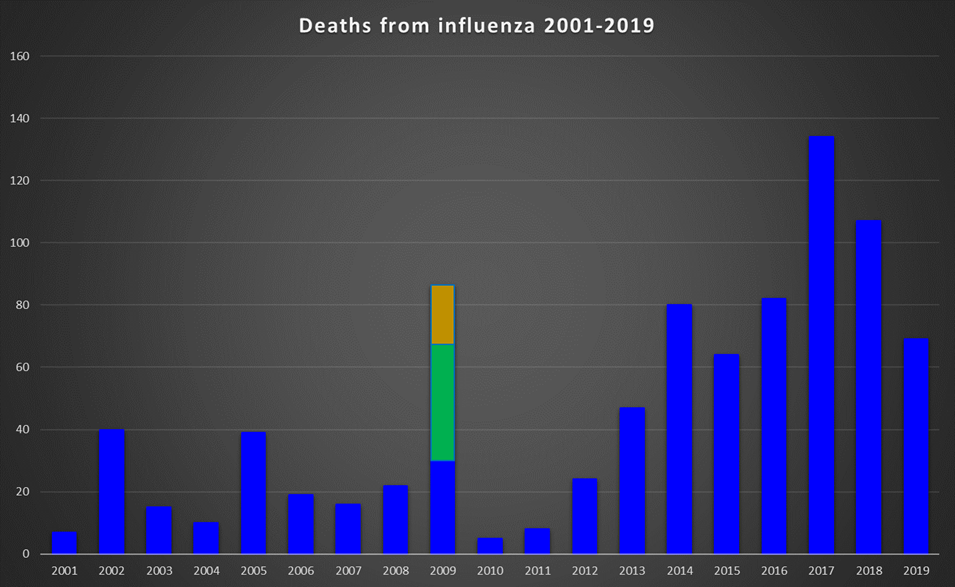
Chart 3: Annual deaths from influenza, 2001 to 2019. Blue bars represent data from the Alberta death database; green and orange indicate additional influenza deaths for 2009 quoted in other Alberta government sources.
Taking this opportunity to dive into a little more detail, Chart 4 shows COVID-19 and flu deaths by year divided into age groups. While the 2009 total flu death toll was not particularly significant relative to other years (using the numbers from the original Alberta government database for consistency), H1N1 was known to be more severe than usual in the younger population. This is apparent in the deaths recorded for the 30-39 age group and to some extent the 20-29-year-olds (Chart 4).
These charts also confirm that for people above age 19, COVID deaths in every age group were considerably higher than flu deaths.
Chart 4: Influenza and COVID-19 deaths by age group, data scaled by annual population
One outcome of the 2009 H1N1 outbreak in Alberta was the expansion of free seasonal flu vaccinations to those individuals not normally at increased risk of serious complications if they contracted the disease, namely the younger and healthier population. Since 2009, the percentage of the population vaccinated has grown steadily; the average over this time period is 27%.[15] This average includes the spike in vaccinations in the two pandemic years, 2009 and 2020, in which 37% of the population was vaccinated.
In 2014, the Alberta government modelled the considerable benefit to society of immunization by graphing the number of hospitalizations expected due to influenza relative to the proportion of the population that was vaccinated for influenza (Chart 5).[16]
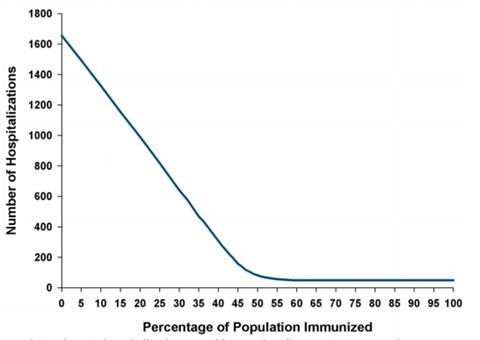
Chart 5: Alberta government model predicting the number of hospitalization relative to vaccinations.
If we scale the actual numbers derived from government data from 2009 through 2019 to the population in 2014 (when the model was produced), we get the real relationship shown in Chart 6.[17][18] Note the change in the y-axis scale to accommodate much higher hospitalizations than expected. Obviously, this is not the ideal outcome, as it appears to show the opposite trend to the model. To their credit, the authors of the model study did offer this helpful definition: “A mathematical model is a simplification of reality that allows users to investigate outcomes across a variety of different scenarios.” “Simplification of reality” indeed – this should be a warning on all scientific models!
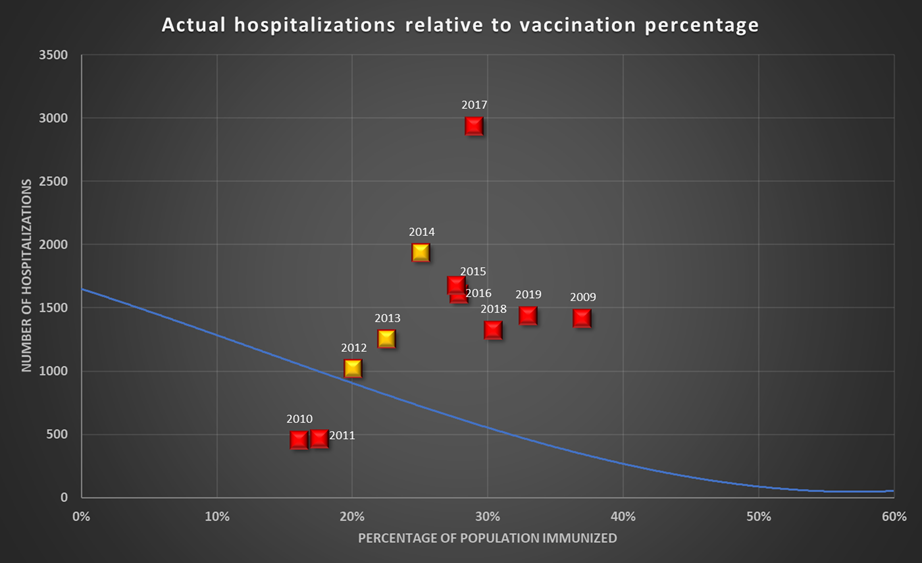
Chart 6: Actual hospitalizations relative to vaccination percentages for the years 2009-2019. Data scaled to the population in 2014. Immunization data for the years 2012, 2013, and 2014 (yellow markers) are estimates based on an extrapolation between 2011 and 2015. Alberta 2014 model shown in blue at chart scale.
Another interesting observation is that contrary to what we might expect, flu deaths in every age group have been significantly greater in the years since 2009 when vaccines became freely available and the proportion of those vaccinated began increasing steadily (Chart 7). For consistency, we are again using the numbers from the original Alberta database, making the assumption that the uncertainty noted earlier in the 2009 data is likely to apply similarly to other death counts.
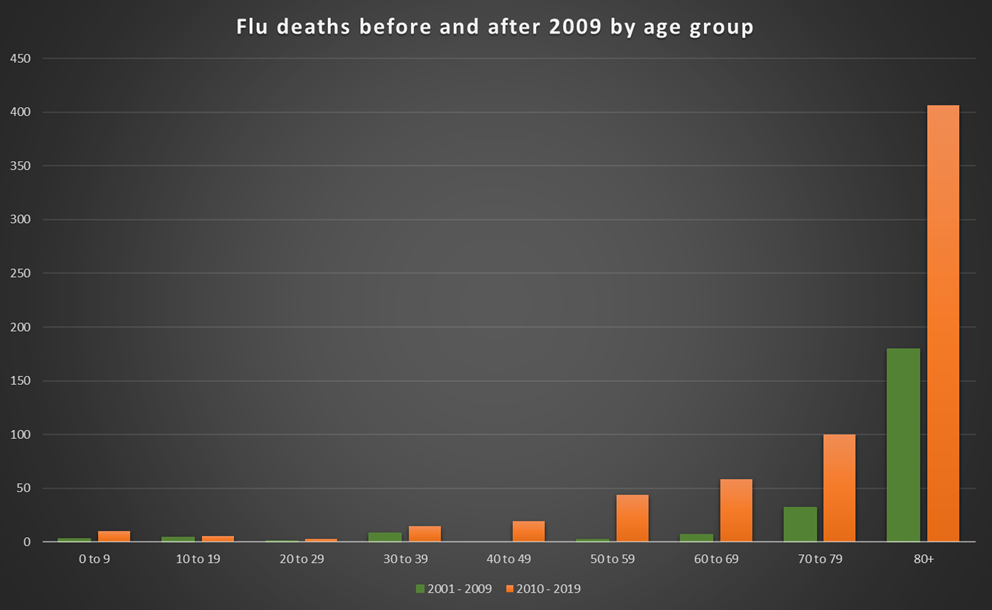
Chart 7: Comparison of flu deaths by age group: 2001-2009 (green) and 2010-2019 (orange).
We should resist jumping to the conclusion from this trend that flu vaccines do not work (or that they make things worse) without additional detailed information about the disease and the deaths. My preliminary investigations show that more severe and unanticipated flu strains have been circulating post-2009. Since decisions regarding the composition of the vaccine need to be made several months in advance of the flu season, in a good year, they are typically 50-60% effective.[19] In years in which one or more unpredicted strains emerge, the vaccines are much less effective.
We know by now that there can be many reasons for anomalous trends in data, and there could be multiple factors at play. Given that the data has revealed these unexpected trends, we can start searching for underlying influences and causes.
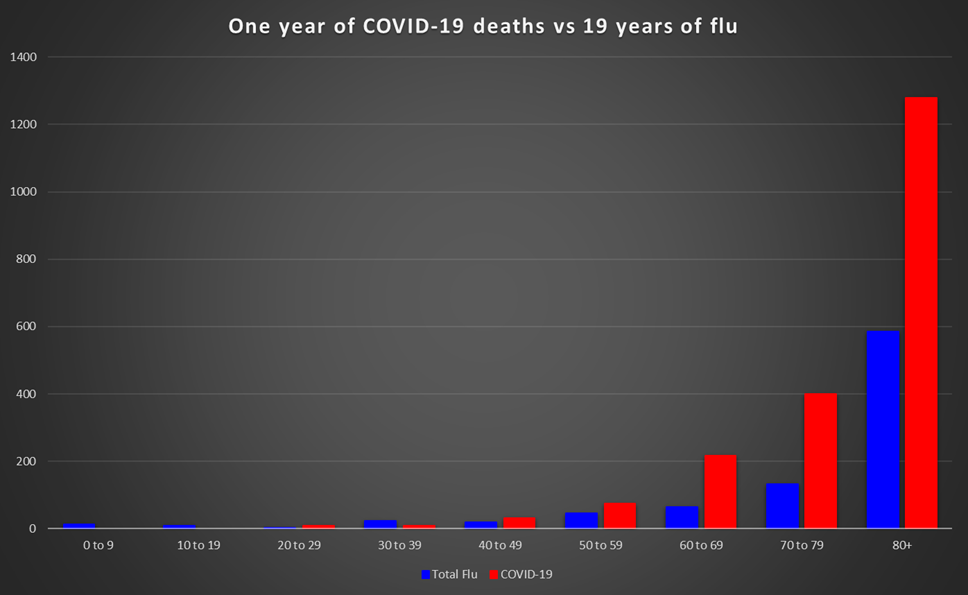
Chart 8: Comparison of COVID deaths in 2020 to the total of all flu deaths from 2001 to 2019 by age group and scaled for population.
After this deep dive into the data, we can say that COVID-19 has had a far more serious impact than the flu – in terms of fatalities – in any of the last 19 years, including 2009, the year of the swine flu. In fact, in most age groups, deaths attributed to COVID-19 in 2020 are significantly greater than the total of all flu deaths from 2001 to 2019 (Chart 8). Meanwhile, an intriguing picture of influenza itself, and the medical understanding and response to it, have emerged from this study, leading us down interesting pathways to greater understanding. From greater understanding, ultimately should come better decisions.
[1] https://open.alberta.ca/opendata/deaths-cause-by-gender-and-age
[2] https://www.albertahealthservices.ca/influenza/influenza.aspx
[3] https://www.who.int/news-room/fact-sheets/detail/hepatitis-c
[4] https://www.merckmanuals.com/en-ca/home/infections/overview-of-viral-infections/overview-of-viral-infections
[5] Ye ZW, Yuan S, Yuen KS, Fung SY, Chan CP, Jin DY. Zoonotic origins of human coronaviruses. Int J Biol Sci. 2020;16(10):1686-1697. Published 2020 Mar 15. doi:10.7150/ijbs.45472 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7098031/
[6] Bodewes R, Morick D, de Mutsert G, et al. Recurring influenza B virus infections in seals. Emerg Infect Dis. 2013;19(3):511-512. doi:10.3201/eid1903.120965 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647654/
[7] Recommended composition of influenza virus vaccines for use in the 2021-2022 northern hemisphere influenza season (who.int)
[8] Ye ZW, Yuan S, Yuen KS, Fung SY, Chan CP, Jin DY. Zoonotic origins of human coronaviruses. Int J Biol Sci. 2020;16(10):1686-1697. Published 2020 Mar 15. doi:10.7150/ijbs.45472 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7098031/
[9] https://www.merckmanuals.com/en-ca/professional/infectious-diseases/respiratory-viruses/coronaviruses-and-acute-respiratory-syndromes-covid-19-mers-and-sars
[10] https://www.who.int/csr/disease/swineflu/frequently_asked_questions/pandemic/en/
[11] https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30484-9/fulltext
[12] https://www.unaids.org/en/resources/fact-sheet
[13] Doshi P. The elusive definition of pandemic influenza. Bull World Health Organ. 2011;89(7):532-538. doi:10.2471/BLT.11.086173 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3127275/
[14] https://open.alberta.ca/dataset/155f4f92-f032-4b9c-b319-738ce8fa2565/resource/52befa08-16d8-436d-9173-60b526412617/download/5584415-2012-review-of-deaths-during-the-2009-influenza-pandemic.pdf
[15] https://open.alberta.ca/publications/2561-3154
[16] https://open.alberta.ca/dataset/f3f8e598-cfe4-4de7-98cb-0a0f18e8babc/resource/e8076707-5ff3-4a2b-ab4b-d13cf6b27d6b/download/hta-2014-03-18-flu-immunization-hospitalizations.pdf
[17] https://open.alberta.ca/dataset/155f4f92-f032-4b9c-b319-738ce8fa2565/resource/52befa08-16d8-436d-9173-60b526412617/download/5584415-2012-review-of-deaths-during-the-2009-influenza-pandemic.pdf
[18] https://www.albertahealthservices.ca/poph/hi-poph-surv-h1n1-ab-experience-2009.pdf
[19] https://www.cdc.gov/flu/vaccines-work/effectiveness-studies.htm
(Laurie Weston – BIG Media Ltd., 2021)