Pandemic-level medical crises have the potential to create intense and widespread pressure on medical systems and personnel, and the COVID-19 pandemic has done so in numerous jurisdictions across the world. Since its arrival in North America early last year, COVID has caused multiple episodes of such pressure on various health-care systems. In North America and many parts of Europe, vaccines are now plentiful and the latest wave of COVID-related pressure on the medical establishment predominantly involves individuals who have chosen not to vaccinate.[1]
Some doctors have expressed frustration with those who have chosen not to receive a COVID vaccine, with a few refusing to see unvaccinated patients on the grounds that they are a danger to others, including medical personnel.[2] [3]Bioethicists have long argued over criteria for prioritizing, delaying, and even denying care in triage. The question of whether being unvaccinated against COVID is a valid reason to be denied care in potentially overstretched ICU facilities in North Texas was recently posed by administration officials.[4]The question has likely been posed elsewhere, or will be.[5]
The idea of denying care to the unvaccinated may appear controversial to many readers. However, the subject of triage – the decision of who gets care and when – in a time of scarce resources is necessarily consequential and controversial. As contentious as these issues may be, they are not new to the ethical study of triage.[6]We will explore the history and principles of triage with an objective approach so that we build the background necessary to understand and assess the subject. What exactly is triage? What are typical criteria used to prioritize patients? Are there criteria that dictate patients may be excluded from care?
The end goal will be a discussion of whether or not – or how and when – vaccination status is relevant in triage.
What is the process of triage?
Triage is commonly performed in emergency departments across Canada and the United States, usually by a triage nurse. It is used to determine prioritization of care. However, triage is not ad hoc or random. It is a process, and there are three requirements for the process to be properly called triage: [7]
- A scarcity of medical resources relative to the number of patients, such that not every patient will receive immediate care. In extreme cases of scarcity, some patients may receive no care.
- A health-care worker (triage officer) assesses every patient’s medical needs based on an examination.
- The triage officer uses a set of criteria to determine the treatment or treatment priority of each patient.
There are several meta-factors affecting the process of triage. The first is the nature of the scarcity, and the second and most contentious is the criterion that is used to determine treatment and priority.
Medical scarcity in a pandemic
Triage is about distributing medical resources, and is only relevant if those resources are at least somewhat scarce. Scarcity exists to a small degree in most hospital emergency departments where not every patient can be treated immediately.[8]The type of triage depends on the nature of the scarcity and the positioning of the patient in the medical system. For example, emergency department triage differs from ICU triage, where the patient has already been admitted to the hospital. The degree and nature of the scarcity of resources is also critical. Triage in a battlefield is different from triage relating to a multicausality car accident, or from a pandemic. Pandemic triage has the potential to be very stressful on entire systems because the medical scarcity is more likely to be far reaching, across jurisdictions, and it may be difficult or impossible to alleviate the lack of resources by transferring patients to locations with lower medical demand.[9]
Focus of care
Triage involves a change in the focus of care, particularly where scarcity of medical resources is severe. In a public health emergency, there is a shift in focus from doctor-patient advocacy on an individual level toward the common or community good. In such circumstances, a statistical estimate of saving the most lives or doing the most good becomes the dominant concern.[10]
Biomedical ethics
While the criteria for treatment priority are specific and contentious, the general principles upon which such guidelines may rest are largely agreed upon. [11]They are:
- Autonomy – the patient has the right to make choices regarding their own health care.
- Nonmaleficence – this is the principle to first do no harm as stated in the Hippocratic Oath. Doing no harm includes ensuring that patients do not wait too long for treatment, as this may result in both direct and psychological harm. [12]
- Beneficence – this is the promotion of good and the removal of harm through direct and beneficial action.
- Justice – is the ideal that resources will be distributed fairly or equally, and that all lives are equally valuable. This is also termed distributive justice.
Applying these principles in practice revolves largely around defining the ideal utility of beneficence to the largest number of patients, while not violating the other principles. Given the exigencies of a disaster or pandemic scenario, defining the decision framework may be challenging, and some patients may suffer.
Prioritization criteria
The criteria for prioritizing patients in triage may fundamentally rest on the principles of biomedical ethics, but it is also dependent on circumstances. Triage was developed in the Napoleonic wars, and either prioritized the preservation of manpower or on treating those patients who could most quickly return to the battlefield. In the context of military conflict, returning to the battlefield was considered by some administrators to be of the greatest good to the community.[13]
For the COVID pandemic, we are most concerned with ICU triage. However, we will examine the other triage criteria for perspective.
Disaster triage
Disaster triage and emergency department triage are very similar. For illustrative purpose, we will look at disaster triage through elemental logic. Patients can be divided into three groups:
- Patients who will die even if treated
- Patients who will likely live, even if untreated
- Patients who will likely live if treated, but die if they are not
The last category gets priority as it results in the most live patients.[14]
Emergency department triage
The criteria for patient prioritization in the emergency room focuses on the severity of illness in the patient. Most countries have either a three-level or five-level scale, in which 1 is the most severely ill and requires the most urgent and timely care, and the higher number of the scale is less urgent and therefore does not require treatment as quickly.[15]
ICU triage
ICU triage is the most relevant type of triage in a pandemic, and COVID has been no exception. During the COVID pandemic, a temporary shortage of ICU beds has been discussed in numerous regions.[16] [17]Although most ICUs appear to function most efficiently at between 70% and 90% capacity, this leaves little reserve capacity for a pandemic. The nature of COVID places strain on one type of equipment (respiratory), which creates a bottleneck of its own.[18] [19]
The question of getting an ICU bed or a ventilator in a scarcity situation becomes a balance between needing it enough (being severely ill) and not having so poor a prognosis that the use of scarce equipment is deemed futile. As in all other triage scenarios, maximizing benefits underlies the criteria. This principle can distinguish between two patients, both of whom will die without ICU facilities, but where one would statistically require the facility for a longer term than the other, and might therefore be denied (or excluded from) care. ICU triage for COVID has specifically been discussed and prioritizes short- or long-term prognosis, life expectancy, and quality of life.[20]
Using short- and long-term prognosis, life expectancy, and quality of life as prioritization criteria is consequential. It brings into play various ethical conundrums such as agism and ableism, and calls into question the principle of justice. Such a conflict of principles, between beneficence and justice, is inevitable given sufficient scarcity. A more complex combination of these terms, called frailty, is sometimes used for this prioritization.
Frailty
ICU triage decisions concern the severely ill and are inherently prejudicial. Judgements must be made about who is too well for ICU level care, and whose prognosis is too poor for the use of the scarce resources. Patients who are very likely to die regardless of care may be excluded under the argument that the use of the scarce resource on them is “futile.” The determination for ICU admission is therefore complex and consequential. It may also lack consistency between locations.[21]
In France and Italy during the first wave of the COVID-19 pandemic, age limits were placed on patients being allowed into the ICUs. This led to widespread public controversy. [22] Several U.K. guidelines suggested that instead of simply using age as a cutoff for ICU exclusion, clinical frailty might be more suitable. Models of clinical frailty may consider these factors:[23] [24] [25]
- Age
- Functional autonomy scale, where a value of 1 is very fit, and 9 is terminally ill
- Co-morbidity, the number of them and their severity
The idea of frailty is to define a medically based heuristic to stand in for the likelihood of adverse outcomes. In numerous studies, frailty is correlated quantitatively or qualitatively with several variables including: life expectancy or mortality, futility, length of ICU stay required (or use of the scarce resource), and post-ICU quality of life. A cartoon, below, illustrates the concept of frailty as a multivariate predictor of chance of death under acute stress, such as ICU-severity COVID.[26]
The use of such methods as a frailty number to make ICU triage decisions may be both unsettling and necessary. This is unsettling because we are balancing values, and the lives and well being of individuals will be affected. This may be necessary because in scenarios of severe scarcity of resources, decisions must be made to preserve the most good.
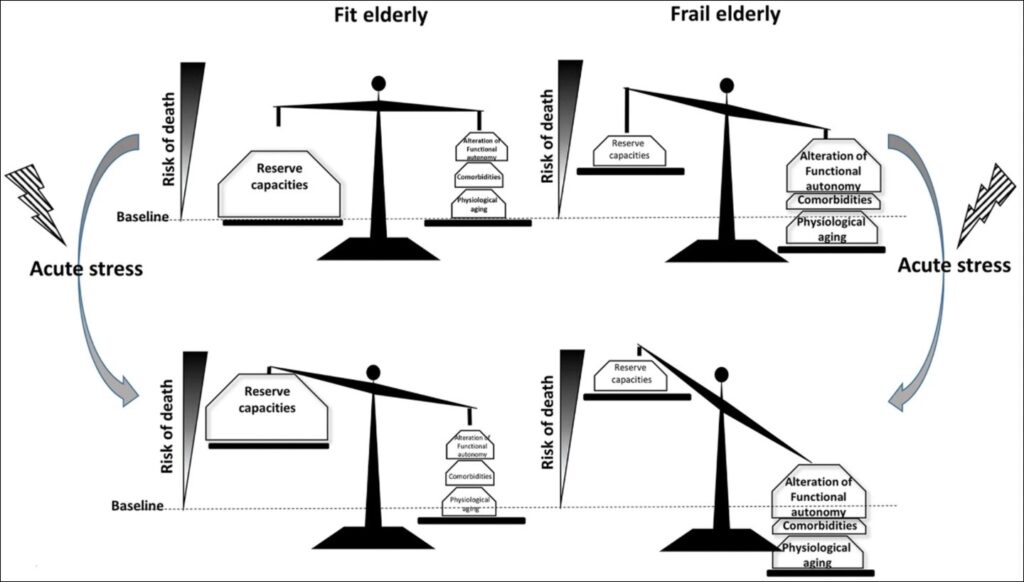
Image reproduced from the open-access article by Guidet et al. “Impact of acute stress on fit or frail elderly. Physiological aging, comorbidities and functional dependency are the main components of frailty syndrome, leading to a decrease in reserve capacities.” The chance of death increases materially when acute stress is introduced, particularly in the frail elderly.[27]
Is vaccination status relevant to triage?
It is notable that the principle of autonomy is fundamental to biomedical ethics. This is relevant to the frustrations over those who have not been vaccinated against COVID. Should the unvaccinated be coerced into vaccinating? While stress on ICU departments is predominantly from the unvaccinated at this time, and there is arguably great beneficence in getting as many people vaccinated as possible, the autonomy principle would not support coercion. It is in the nature of principles that the so-called easy answers are often complicated. Practitioners are directed to think carefully.
What about doctors who say they will not treat the unvaccinated? Refusing to treat a patient based on vaccination status might be a violation of the Hippocratic Oath, or the nonmaleficence principle, since denial of care is, in fact, a harm. However, the evaluation of this question has nuance. Choosing to treat the unvaccinated outside of the physical clinic may not be unethical from the perspective of protecting other patients. However, ethical judgement rests on the true motivation of the policy. Is such a decision punitive or is it actually to protect other patients?
Could the unvaccinated be denied access to an ICU bed? Yes, under some circumstances, though it may not be directly because they are unvaccinated. If there exists too great a shortage of ICU facilities, unvaccinated ill patients may not be treated in the ICU simply as part of the standard triage criteria. The greater the number of severely ill patients there are, the more likely this could be. Further, the mortality rate of severely ill COVID patients will be considered in choosing treatment. If unvaccinated persons were deemed by the triage officer as less likely to survive than others, they could rationally be excluded from treatment.
The autonomy principle has been cited in the evaluation of liver-transplant candidates as an argument not to exclude patients solely based on alcohol and drug dependencies. Alcoholism is clearly relevant from the evaluation of outcome and beneficence, but it is questionable and controversial as a sole factor for exclusion. Being unvaccinated is not as relevant to ICU outcome as the liver example in transplantation. The point here is that the autonomy principle clearly states that medical systems should not judge patients based on the decisions they make for themselves, even if the practitioner disagrees with the concept. The principle of justice would also likely be violated in the case of the unvaccinated being denied treatment.[28]This leaves the argument to treat the unvaccinated differently on thin moral ground, entirely dependent on a hypothetical mortality-rate argument.
This discourse on triage has necessarily focused on the ethical obligations of practitioners in the medical system. During a pandemic, tough decisions may be made on which patients to treat first, or in the worst scenarios, which to treat at all. In accordance with the principles behind common health-system standards, vaccination status should not be a factor in triage decisions.
[1] Hunt, Lee, September 21, 2021, BIG-Media.ca, Taking a long-term view of the decision to vaccinate
[2] Bains, Camille, September 3, 2021, Doctors frustrated with ‘selfishness’ of anti-vaccine protestors, people unvaccinated against COVID-19, The Globe and Mail, Doctors frustrated with ‘selfishness’ of anti-vaccine protesters, people unvaccinated against COVID-19
[3] Bella, Timothy, September 7, 2021, The Washington Post, Florida doctor says she won’t treat unvaccinated patients in person
[4] Teagarden, Russell, August 24, 2021, NBC News, If Covid vaccine refusers are turned away at hospitals and doctors offices, is that ethical?
[5] Wisconsin Examiner, August 29, 2021, Medical Triage: Hospitals face the ethical dilemma of deprioritizing care for eligible unvaccinated people
[6] Shaw, David, June 22, 2020, Triaging ethical issues during a pandemic: a rough guide, Journal of Medical Ethics Blog
[7] Iverson, Kenneth, and John Moskop, 2007, Triage in Medicine, Part I: Concept, History, and Types, Annals of Emergency Medicine, Vol 49, No 3, 275-281
[8] Iverson, Kenneth, and John Moskop, 2007, Triage in Medicine, Part I: Concept, History, and Types, Annals of Emergency Medicine, Vol 49, No 3, 275-281
[9] Iverson, Kenneth, and John Moskop, 2007, Triage in Medicine, Part I: Concept, History, and Types, Annals of Emergency Medicine, Vol 49, No 3, 275-281
[10] Aacharya, Ramesh, Chris Gastmans, and Yvonne Denier, 2011, Emergency department triage: an ethical analysis, BMC Emergency Medicine, 11:16
[11] Beauchamp, Tom, and James Childress, 1979, Principles of Biomedical Ethics, Oxford University Press, ISBN 9780195024876
[12] Aacharya, Ramesh, Chris Gastmans, and Yvonne Denier, 2011, Emergency department triage: an ethical analysis, BMC Emergency Medicine, 11:16
[13] Iverson, Kenneth, and John Moskop, 2007, Triage in Medicine, Part I: Concept, History, and Types, Annals of Emergency Medicine, Vol 49, No 3, 275-281
[14] Kipnis, Ken, 2002, Triage and Ethics, AMA, Journal of Ethics, Virtual Mentor, 2003, Vol 4, No 1
[15] Aacharya, Ramesh, Chris Gastmans, and Yvonne Denier, 2011, Emergency department triage: an ethical analysis, BMC Emergency Medicine, 11:16
[16] Holcombe, Madeline, September 1, 2021, These 5 states have less than 10% of ICU beds left as Covid-19 overwhelms hospitals
[17] Johns Hopkins University and Medicine, Weekly Hospitalization Trends, Sept 20, 2021
[18] Lanese, Nicoletta, July 27, 2020, Live Science, What happens when the ICU is full?
[19] Bean, Mackenzie, August 6, 2020, Becker’s Hospital Review, Two healthcare leaders talk ICU capacity: 5 sound bites
[20] Joebges, Susanne, and Nikola Biller-Andorno, 2020, Ethical guidelines on COVID-19 triage—an emerging international consensus, Critical Care, 24, 201(2020)
[21] Wilkinson, Dominic, 2020, Frailty Triage: Is Rationing Intensive Medical Treatment on the Grounds of Frailty Ethical? The American Journal of Bioethics
[22] Orfali, Kristina, 2020, What Triage Issues Reveal: Ethics in the COVID-19 Pandemic in Italy and France, Journal of Bioethical Inquiry, Vol 17, 675-679
[23] Wilkinson, Dominic, 2020, Frailty Triage: Is Rationing Intensive Medical Treatment on the Grounds of Frailty Ethical? The American Journal of Bioethics
[24] Guidet, Bertrand, et al, 2018, Caring for the critically ill patients over 80: a narrative review, Annals of Intensive Care 8, 114
[25] Netters, Sabine et al, 2020, Pandemic ICU triage challenge and medical ethics, BMJ Supportive and Palliative Care, Vol 11, No 2, 133-137
[26] Guidet, Bertrand, et al, 2018, Caring for the critically ill patients over 80: a narrative review, Annals of Intensive Care 8, 114
[27] Guidet, Bertrand, et al, 2018, Caring for the critically ill patients over 80: a narrative review, Annals of Intensive Care 8, 114
[28] Greenberg, Rebecca, et al, 2021, Canadian Society of Transplantation White Paper: Ethical and Legal Considerations for Alcohol and Cannabis Use in Solid Organ Listing and Allocation, Transplantation, Vol 105, No 9, 1957-1964
(Lee Hunt – BIG Media Ltd., 2021)