As COVID progresses, mutates, and continues to be a dominating presence in our lives, one might begin to focus increasingly on the role of masks in our lives.
In western societies, masks were virtually non-existent in our daily lives before governments began mandating that we wear them. Now, they are everywhere. Some people have embraced mask use, others have been passive, and others resistant. Along the way, how many of us have stopped to research – or even ponder – the science behind masks?
Most of us have seen agenda-driven articles and posts that claim to either categorically prove or refute the effectiveness of masks. We take a different approach here, presenting relevant, scientifically sound research with logical interpretation for you to review. There are many factors involved in assessing the merit of wearing masks amid the COVID-19 crisis including materials, layers, how people wear the masks, and how they behave while wearing masks. In this article, we take a dive into how masks work and let data do most of the talking.
First, there are a few terms on which we should get up to speed in order to better understand mask research:
Hydrophobic: repels/does not mix with water
Hydrophilic: mixes well with water
Filtration efficiency: the percentage of a certain size of particles unable to pass through, or are caught, by a filter medium.[1]
There are three general methods of being infected by an airborne virus, such as that of coronavirus: submicron aerosols, large droplets at high velocities, and macrodroplets (Guha et al, 2021). You can think of submicron aerosols as being extremely tiny viral particles that hang around in the air for a while after being emitted from one’s mouth when talking, breathing, etc. Large droplets are those spit globules you see fly out when someone coughs or sneezes. And macrodroplets as larger nose drops or splashes that land on surfaces and therefore allow transmission of viral particles via direct contact (Guha et al, 2021).
Now, let’s look at your standard surgical mask. Surgical masks, according to the U.S. Food and Drug Administration (FDA) website, can be labelled as “surgical, isolation, dental, or medical procedure masks,” and are meant to block large particle droplets and splashes so they do not reach your mouth or nose.[2] Looking at the structure, according to Wibisono et al (2020), surgical masks are made with a spunbond-meltbond-spunbond method, which provides the highest level of protection. It can protect you from 98% of bacteria and impose hydrophobicity.
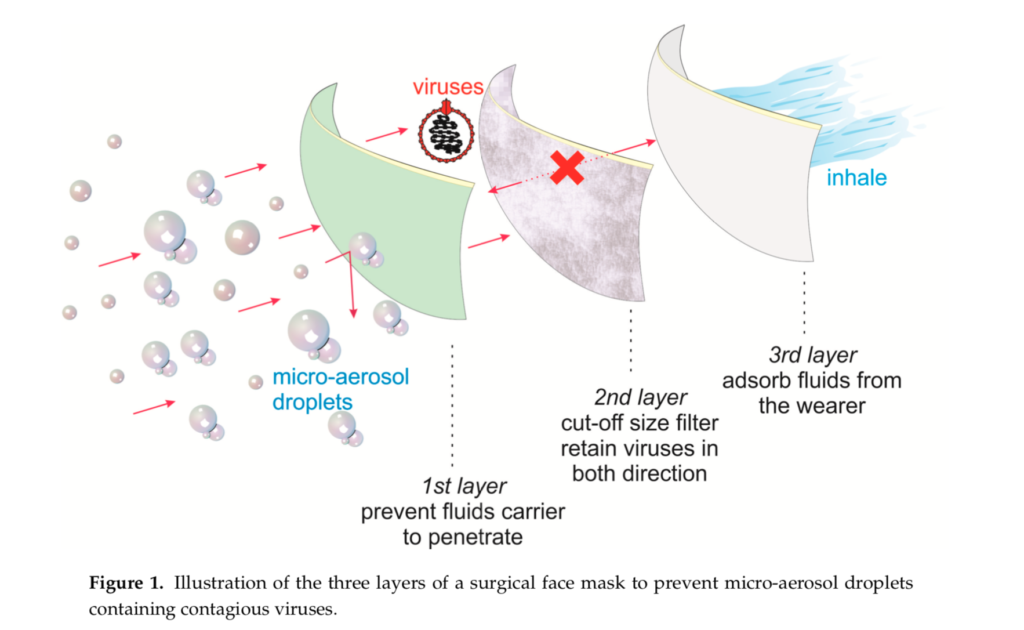
A surgical mask has three layers, each of which serves an important purpose: the outer layer is a hydrophobic layer, the middle layer is a filter, and the inner layer is absorbent, or hydrophilic (Wibisono et al, 2020). The outer layer’s hydrophobic quality repels water droplets that hold viral particles. Within the meltbond technique, a die process allows fine microfibres and a smaller pore size to form the filter layer in a surgical mask (Wibisono et al, 2020). The filter layer retains bacteria and virus particles so they do not reach the inner layer of your mask. And the inner layer is hydrophilic to hold onto any water droplets you breathe out that may contain viral particles or bacteria, or to catch any inbound droplets that may have made it through the other layers of the mask. The inner layer is made to catch viral particles moving through the mask in either direction (Wibisono et al, 2020). It is important to note that surgical masks do not block small particles completely.[3] If you are not sufficiently distant from others, wearing a surgical mask does not stop you from inhaling small particles; that is not its purpose. Rather, it is intended to block splatters.
Another type of mask relevant to COVID-19 is the N95. An N95 is not actually classified as a mask, but as a respirator.[4] Simple respirators, as in the case of the N95, act to “filter out airborne particles,” whereas a mask acts to simply block particles.[5] The “N” denotes that this respirator is “not resistant to oil,” and the “95” indicates that the “respirator is capable of filtering out 95% of particulate matter that is 0.3 microns or larger.”[6]The N95 respirator must form a seal on your face, thereby not allowing entry or exit of air particles except through the respirator.[7] An N95 has the same three basic layers as a surgical mask: an outer, inner, and filter layer (Wibisono et al, 2021). A big difference, however, is that the N95 has layers within its layers. The outer, hydrophobic layer consists of two layers; the filter layer is still a single layer, but the inner, hydrophilic layer is composed of seven or eight layers (Wibisono et al, 2021). The pore size of the N95 filter is around 300 nanometres (Wibisono et al, 2021), and the particle size of coronavirus ranges from 60 to 140 nanometres (Rowan & Moral, 2021). This, of course, means that the coronavirus particles are small enough to fit through the pores in the filter of the mask – meaning that not even the N95 mask is 100% effective.
After looking at surgical masks and N95 respirators, we have a basic understanding of how masks are designed and how they are intended to work. Now, we can examine the most commonly used face covering – the cloth mask. A 2021 study examined the results of how 21 different materials performed with the three aspects of infection: submicron aerosols, large droplets (at high velocities), and macrodroplets (Guha et al). Looking at the submicron aerosols, Guha found that only five fabrics presented a dry filtration efficiency of more than 30%. In comparison, a surgical mask is normally required to have a filtration efficiency of at least 80% (Wibisono et al). All five of those fabrics were tightly woven. If cotton, they had to be high on reported threads per inch. Even with this, those fabrics achieved 40-50% filtration efficiency for submicron aerosols (Guha et al, 2021). The researchers looked at large droplets at high velocities in order to simulate a cough or sneeze. Sneezes can reach velocities up to 1,700 centimetre/second (Guha et al, 2021). That is equivalent to 61.2 kilometres per hour, which is considerably faster than Usain Bolt’s top sprint speed of 44 km/h, so good luck evading the spit from your friend’s sneeze. Your only hope is if you bail out on the windup.
In order to simulate the range of droplets produced by coughing, the researchers generated aerosols with a range of 0.5-20 micrometres, and found that both 1,000-thread-count pillowcase and cotton flannel had typical efficiency levels for filters in relation to size. They also found that, surprisingly, a 100% microfiber polyester bandana mask had wet filtration efficiency greater than 99% across all cough particle sizes (Guha et al, 2021). They theorized that the high filtration efficiency of the polyester bandana was a result of its hydrophobic properties. Essentially, Guha et al found that the majority of materials had more than 90% droplet filtration efficiency, meaning cloth masks fare quite well in protection against larger droplets from sneezes and coughing. Guha et al used macrodroplets as the third test criteria because after bouts of frequent coughing, fluid can build up on the inner surface of a mask, eventually forming droplets that permeate to outer layers because of saturation, and may drip. They found that most single-layer materials failed the criteria, and even with some triple-layer materials, there was some failure in a permeability test. Therefore, cloth masks should have at least three or four layers (Guha et al, 2021). Another 2021 study looked at the efficacy of cloth masks, and found that in comparison to a medical mask that has a 44% particle penetration, cloth masks have a 97% particle penetration (Rowan & Moral).
It seems to be said that the best cloth masks have three or four layers, ideally composed of three different materials, one for each purpose (hydrophobicity, filtration, and hydrophilicity), and if using cotton, make sure it is tightly woven. This all said, cloth masks will not filter out submicron aerosols, as this is not their intended use. If you are looking for basic coverage, the polyester bandana seems to have value beyond robbing banks and showing your gang colours; it performed well in studies for a simple cloth mask.
After deciding what material to use for your cloth mask, the World Health Organization recommends reuse. The instructions given are to wash with soap or detergent in water greater than 60 degrees Celsius or to wash in room temperature water with soap or detergent and then boil for 1 minute at least once a day.[8] One group of researchers that tested mask durability with repetitive washing found that after the fourth washing, the pore size of the mask increased, thereby causing the filtration efficiency to decrease by 20% (Wibisono et al). A separate group of researchers found the same 20% decrease in filtration efficiency after four wash and dry cycles (Rowan & Moral, 2021). Essentially, the more cloth masks are used, the less effective they become.
To summarize, there is a clear ranking in protection from COVID-19 – wearing an N95 mask, then a surgical mask, then a cloth mask. We know COVID-19 can be released in submicron aerosols that linger in the air, and surgical and cloth face coverings are not made to protect you against such particles. They might reduce the amount of particles that reach your face, but it is important to remember that surgical and cloth masks are made to block splashes of larger droplets. We also know there is a hierarchy of materials when using cloth masks. If you are going to wear a cloth mask, it makes sense to wear one with three layers, find the right materials, and, obviously, wear it properly. To those wearing a balaclava, or any material with holes cut for ease of breathing – the only protection offered is that no one will want to be anywhere near you.
There is an abundance of scientific research on masks, and there are countless variables regarding efficacy in a pandemic. This article was a look at the basics; we will look at related topics in future stories. Feel free to leave a comment about mask research or a related story angle, dataset, or report that you believe is particularly noteworthy.
Guha S, Herman A, Carr IA, Porter D, Natu R, Berman S, et al. (2021) Comprehensive characterization of protective face coverings made from household fabrics. PLoS ONE 16(1): e0244626. https://doi.org/10.1371/journal. pone.0244626
Rowan, N. J. & Moral, R. A. (2021) Disposable face masks and reusable face coverings as non-pharmaceutical interventions (NPIs) to prevent transmission of SARS-CoV-2 variants that cause coronavirus disease (COVID-19): Role of new sustainable NPI design innovations and predictive mathematical modelling. Science of the Total Environment 772. https://doi.org/10.1016/j.scitotenv.2021.145530
Wibisono, Y., Fadila, C. R., Saiful, S. & Bilad, M. R. (2020) Facile Approaches of Polymeric Face Masks Reuse and Reinforcements for Micro-Aerosol Droplets and Viruses Filtration: A Review. Polymers 23(2516). https://doi.org/10.3390/polym12112516
[1] https://www.sciencedirect.com/topics/engineering/filtration-efficiency
[2] https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks
[3] https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks
[4] https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks
[5] https://www.cdc.gov/niosh/topics/respirators/default.html
[6] https://www.csagroup.org/wp-content/uploads/CSA_Medical_PPE-FAQs_Digital.pdf
[7] https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks
[8] https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-masks
(Skye Thompson – BIG Media Ltd., 2021)