“Breathe,” the pleasant voice advised as I floated in and out of consciousness in the recovery room following ankle surgery on May 24. I had stopped breathing, a condition called apnea, which is not uncommon following anesthesia or anesthesia with opioids. This happened again and again. Sometimes I was aware of my breathing stopping, hovering on the edge of consciousness, I would feel myself … just … stop … breathing. Other times, I would startle awake and consciously force a deep breath. Sometimes I would fail, and the nurse would say once more, “Breathe.”
I looked at her, and smiled, acknowledging her, noting that she sat at a small, pedestal-style workstation, watching my oxygen stats and other data. Sometimes I would open my eyes and find her staring at me. She was watching me with an unerring focus, making sure I kept breathing. Although the anesthetic still in my system is known to affect the formation of memory, I knew I would never forget this nurse’s intense focus on my well-being.
This was a strange state of mind and body. Anesthesia is meant to take control of the autonomic nervous system from the patient, among other things, and opioids affect breathing patterns in numerous ways.[1]This affect on breathing is one of the reasons that the opioid crisis has been so deadly. Here I was in the hospital, somewhat aware of what was going on, yet only partially in control of mind and body, definitely not in autonomic control of my breathing. But I had a guardian, and her eyes were on me.
“Breathe,” she said again.
I did breathe, but some part of me stored this experience away and wondered how different my situation would be if I had imbibed opioids of unknown dosage and mix on the street, away from such excellent and conscientious care.
What anesthesia is meant to do
The goals of anesthesia are to create a reversible coma that will allow surgery to be accomplished with the best outcomes for the procedure and the patient. Anesthesiologists agree that to do so, there are key, measurable goals that the anesthetic agent must achieve.[2][3]They are:
-
- To render the patient unconscious, effecting a state of amnesia or oblivion over the experience of the surgery.
- To gain control over the autonomic nervous system (ANS).
- To immobilize the patient.
These key goals are illustrated in the image below, as a triangle, adapted from a journal depiction by Egan and Svensen.[4]The importance of the third goal – immobilization – is the easiest to intuit, as the patient must hold still to avoid interfering with the surgery. The components of the first goal – unconsciousness and amnesia – are associated with the psychological stress on the patient, during and after surgery. The middle goal – control of the ANS – is the least obvious but just as important. Consider that the role of the ANS is to compensate and modulate bodily functions based on environmental and stress factors. This includes heart rate and breathing. Control of the ANS during surgery is critical so that ANS compensation to the stress of surgery does not harm the patient.[5][6]
Anesthetics have a crucial role in surgery, and these three goals are far from simple to achieve, especially as they represent a profound interference with the patient’s mental and physical state, right to the unknowing responses of the ANS, including breathing and heart regulation. To have these precise and profound effects and yet be reversible, is asking for much, and the discussion over the best pharmaceuticals to use in anesthesia continues.[7]
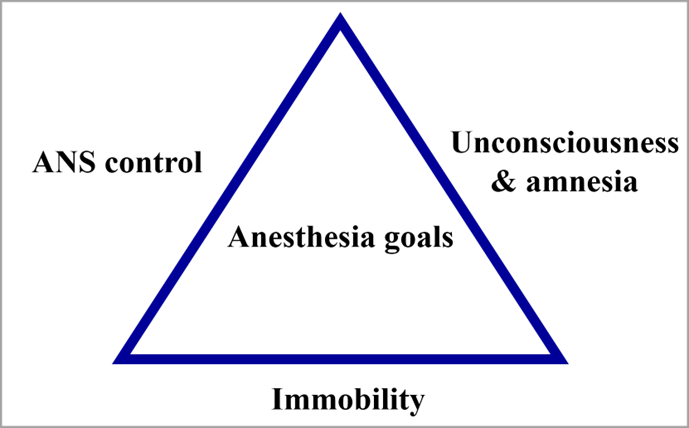
Goals of anesthesia. Adapted from Egan and Svensen.[8]
Why opioids are used
Opioids, including fentanyl, are commonly used in anesthesia – so commonly that the question is sometimes asked by anesthesiologists as to whether surgery can even be done without opioids. While anesthesiologists will agree that surgery can be accomplished without opioids, they do fulfill a vital role, and the conversation around reducing their use is challenging, even in the face of an opioid-misuse crisis.[9][10]
No single drug is capable of achieving all three goals of anesthesia, except perhaps in very high (and inadvisable) quantities. Opioids effect all three goals, particularly ANS control, and ANS responses to stress and pain from surgery. Further, when opioids are used in conjunction with other agents, the overall concentrations of anesthesia drugs are significantly reduced. The use of opioids during surgery are well supported from this perspective, though the concerning misuse of them after surgery must be addressed.[11]
Harms from opioids
There are side effects from opioids, which are well known. These include nausea and constipation, apnea, grogginess, and dizziness.[12][13][14]
But these side effects are minor compared to their benefits when opioids are used correctly, and are not really what we refer to when we use the word “harms”. One of the biggest harms of opioids is that they create a state of euphoria and are addictive.[15][16][17][18]
The very power of opioids in controlling the ANS, so useful in surgery, can also unfortunately suppress autonomic functions in the brain and nervous system to the point where patients stop breathing entirely. Their bodies do not even know they need to breathe as they asphyxiate.[19]
The opioid crisis
Much has been written about the massive increase in misuse of opioids in North America, and its roots in prescribing opioids for pain or for post-surgical use. Overdose is now the leading cause of preventable death in the United States with over 2.4 million U.S. residents deemed to have a severe opioid-use disorder.[20]The reasons for this crisis are complex, not limited to prescribing patterns, and go beyond this article. This said, my recent medical experience seemed rife with examples peripheral to the problem.
Prior to my surgery, I was given materials by Alberta Health Services regarding pain management and opioids.[21]Being aware of the opioid crisis, I took note of one particular page of the document suggesting that addiction is unlikely if these drugs are used as directed. A portion of that page is reproduced below. The advice in this page appears rational and reasonable. However, given the rampant misuse of opioids in North America, it was noteworthy.
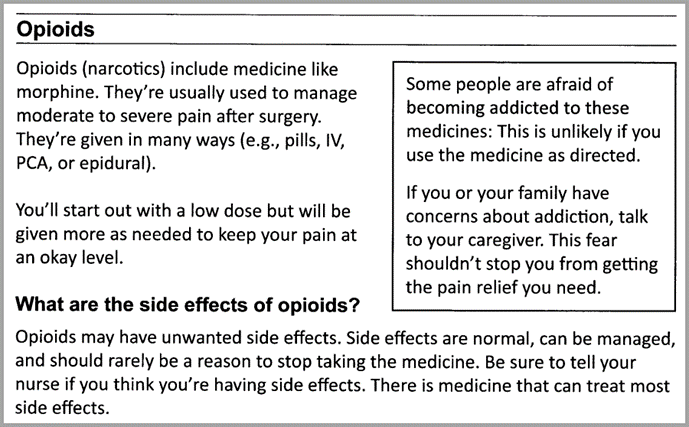
An excerpt from the Alberta Health Services “Managing Pain after Surgery” document I was given prior to ankle surgery.[22]
Deaths due to opioids
The Government of Canada recently accumulated data related to opioid toxicity deaths in Canada, with special concerns regarding the effects of the COVID pandemic and associated changes in social behaviours during that period. For that reason, the report was organized to isolate the first three quarters of 2020, when the pandemic began, versus the same periods of time in previous years and in 2021.[23]
We show the results of this report for deaths ruled accidental (rather than suicide or undetermined) in the chart below. The deaths given are suppressed to some degree by factors particular to each province (Quebec, for example, does not publish data for opioid deaths for individuals under the age of 20). Undetermined drug-related deaths are also not included. This means the true rate of accidental opioid deaths is higher than the chart shows.
Some other pertinent findings from the study:[24]
-
- Opioid misuse kills more males than females (74% of the deaths were men from January through September 2021)
- The majority of opioid deaths are among individuals aged 20-59
- 86% of opioid deaths involved fentanyl
- 82% of opioid deaths involve drugs with a non-pharmaceutical source
While the report writers concluded that there was a 95% increase in opioid deaths in the first year of the pandemic compared to the previous year, readers might note that a trend line of increasing opioid deaths could have been drawn from 2016 to 2021, with a dip in 2019. This interpretation could be supported in the data, however the causality of increased deaths of this kind during the pandemic has been supported by other sources, such as in this article Analysis of excess deaths in 2020 reveals surprising deviations on excess deaths in Alberta, and this article on overdose deaths COVID collateral – overdose data shows alarming crisis.
In the former report, a significant number of excess deaths in 2020 among males were shown to be due to accidental drug and alcohol toxicity.
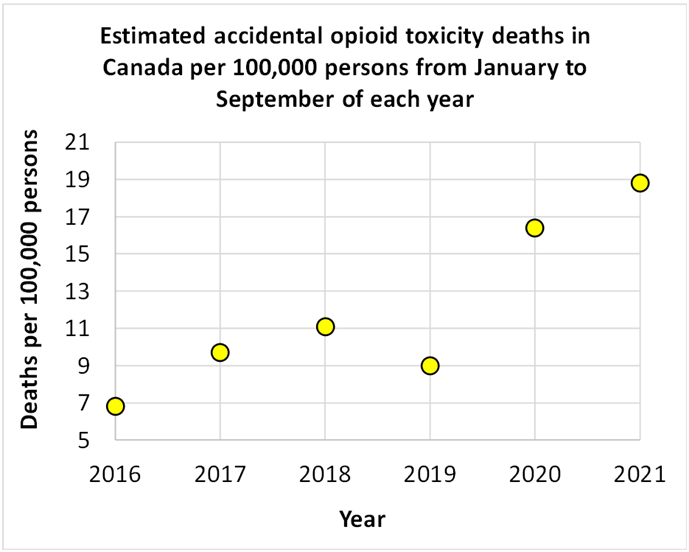
Estimated accidental opioid toxicity deaths in Canada per 100,000 persons in the first three quarters of 2016 to 2021.[25]
How did we get here?
I know how I ended up in surgery and the recovery room. I am a rock climber. And as I described in this article In search of the zone on the sharp end, I climb to find a state of optimal mind-body performance. It was of some irony that shortly after writing an article about human achievement that I was to injure my ankle climbing, tearing my peroneal tendon, spraining other parts of my ankle, and rupturing my superior peroneal retinaculum. I chose to find a positive way to look at my injury, and described that process in this article, When failure is not failure: the rationality of positivity amid catastrophe.
Some victims of the opioid crisis became addicted to opioids after accidents. The recent Government of Canada report suggests that social factors associated with the COVID pandemic have had a material effect on the opioid crisis. We cannot hope to do more than start a conversation on the subject of opioids or addiction in this article, but we might take note that these awful and life-changing situations are never far away from us.
After all, there I was in the recovery room after my surgery, struggling to breathe normally due to the opioids in my anesthesia.
We are all in a room somewhere
I felt the power of the drugs in my inability to breathe. It is worth noting that the power of the opioids also helped enable what appears to be a successful operation on my ankle. But lying there, feeling my chest fail to inhale, I had a glimpse of an ineffable helplessness. These drugs have the power to end human life abruptly.
And I knew that there was something new for me to think about. Thankfully, I had a caring and conscientious guardian watching me breathe while these thoughts burned themselves into my perception. If only we could all be so fortunate.
References
[1] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[2] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[3] Egan, Talmage and CH Svensen, 2018, Multimodel general anesthesia: a principled approach to producing the drug induced, reversible coma of anesthesia, Anesth Analg. 2018; 127: 1104-1106
[4] Egan, Talmage and CH Svensen, 2018, Multimodel general anesthesia: a principled approach to producing the drug induced, reversible coma of anesthesia, Anesth Analg. 2018; 127: 1104-1106
[5] Savvina, Irina, et al, November 30, 2021, General Anesthesia and Autonomic Nervous System: Control and management in Neurosurgery
[6] Paloheimo, M. P. J., et al, 2010, Autonomic nervous system state: the effect of general anaesthesia and bilateral tonsillectomy after unilateral infiltration of lidocaine, British Journal of Anaesthesia, V 104, 5, p587-596
[7] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[8] Egan, Talmage and CH Svensen, 2018, Multimodel general anesthesia: a principled approach to producing the drug induced, reversible coma of anesthesia, Anesth Analg. 2018; 127: 1104-1106
[9] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[10] Ferry, Nicholas, and Sandeep Dhanjal, March 28, 2022, Opioid Anesthesia, National Library of Medicine
[11] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[12] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[13] Egan, Talmage and CH Svensen, 2018, Multimodel general anesthesia: a principled approach to producing the drug induced, reversible coma of anesthesia, Anesth Analg. 2018; 127: 1104-1106
[14] Ferry, Nicholas, and Sandeep Dhanjal, March 28, 2022, Opioid Anesthesia, National Library of Medicine
[15] Egan, Talmage, 2019, Are opioids indispensable for general anaesthesia? British Journal of Anaesthesia, V 122, 6, p127-135
[16] Egan, Talmage and CH Svensen, 2018, Multimodel general anesthesia: a principled approach to producing the drug induced, reversible coma of anesthesia, Anesth Analg. 2018; 127: 1104-1106
[17] Ferry, Nicholas, and Sandeep Dhanjal, March 28, 2022, Opioid Anesthesia, National Library of Medicine
[18] Maron, Dina Fine, January 8, 2018, How Opioids Kill, Scientific American
[19] Government of Alberta, Alberta Health Services, Managing Pain after Surgery
[20] Vashishtha, Devesh, et al, 2017, The North American opioid epidemic: current challenges and a call for treatment as prevention, Harm Reduction Journal
[21] Government of Alberta, Alberta Health Services, Managing Pain after Surgery
[22] Government of Alberta, Alberta Health Services, Managing Pain after Surgery
[23] Government of Canada, March 2022, Opioid- and Stimulant- related Harms in Canada, https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
[24] Government of Canada, March 2022, Opioid- and Stimulant- related Harms in Canada, https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
[25] Government of Canada, March 2022, Opioid- and Stimulant- related Harms in Canada, https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
(Lee Hunt – BIG Media Ltd., 2022)