The continuation of the COVID-19 pandemic is causing new levels of frustration amongst the populace, including among health care professionals. That frustration centres on the question of vaccination, in particular where uptake of vaccination is low, but vaccines are readily available.
The United States has a 54% reported rate of full vaccination relative to its entire population, while Canada has 69%, and Europe has 51%. The global rate is 31%.[1]In the U.S. and Canada, vaccines are widely available. Many of the vaccinated, including some North American medical officials have expressed frustration over the unvaccinated.[2] [3]
Vaccine passports have been introduced or discussed in many parts of the world, sparking spirited debate over the ethics and morality of such a measure. Recently, the Alberta provincial government announced a $100 gift card to individuals who choose to fully vaccinate.[4] [5]
While the ongoing nature of the pandemic is unfortunate, it can be understood both from an epidemiologic and a decision-making perspective. An understanding of both may be helpful to readers. Further, greater certainty and acceptance of our situation may result in more rational policies and calmer outlooks.
Key facts as we understood them in the past
- As reported in BIG Media article Understanding vaccine effectiveness and breakthrough, the Delta variant may be transmissible in breakthough cases from the vaccinated.[6]
- As reported in another BIG Media story Predicting vaccination rates and outcomes for the Delta variant, herd immunity may be difficult to achieve for the Delta variant given imperfect vaccination effectiveness. An effectiveness of at least 80% is required for herd immunity to be mathematically possible for Delta.[7]
This is why BIG Media suggested on Aug. 16 that “Even under simple, optimistic models, Canada’s current vaccination levels will not prevent a fourth wave of COVID-19 driven by the Delta variant.”
Are the vaccine hesitant irrational and/or arrogant?
Frustration toward the unvaccinated have boiled over for some. Many politicians and medical officials have stated that they believe the decision to avoid vaccination for COVID-19 is selfish and puts lives at risk.[8] Besides the question of whether such comments are unhelpful, are they rationally justified? Can the issues of vaccine hesitancy be understood in more productive and reasonable terms?
In this article Prisoner’s dilemma and vaccination, we described the game theoretic decision process to vaccinate as a payoff formula between the relative risks of vaccination versus infection and the chance of infection.
where m is the relative risk of vaccination over infection, and pv is the probability of infection, which drops with higher rates of vaccination. At high rates of vaccine uptake, the payoff to vaccinate decreases and societal co-operation (not in the formula) becomes important.
If this rational framework is correct, the decision to vaccinate or not comes down to several factors, particularly to the perception of relative risk and the probability of infection. It has been shown in previous studies that the perception of vaccine risks, that is side effects from the vaccine, tend to be inflated.[10] Moreover, the game theoretic expectation from a vaccine scare is to materially affect vaccine uptake. [11]
A rational, and non-pejorative, response to the vaccine hesitant is therefore to discuss the real versus perceived relative risk of vaccinating or not. Calm is required here, not abuse. An update of the continuing chance of infection relative to vaccine effectiveness and the herd immunity chart may also be useful in the vaccination decision.
Different measures of vaccine effectiveness
Vaccine effectiveness is also relevant in this discussion and needs to be updated. In the article Understanding vaccine effectiveness and breakthrough, we defined vaccine effectiveness. It is a relative measure, defined as “The percentage reduction in the incidence of disease among vaccinated persons compared with unvaccinated persons.”[12]We also said that the term vaccine effectiveness can be expanded to mean several things, including the effectiveness against severe outcomes such as hospitalization or death.
In epidemiolocal studies, this expansion can also include the notion of transmissibility (infectiousness) separately from susceptibility.[13]In this case, susceptibility refers to whether the disease causes severe symptoms (morbidity). The total vaccine effectiveness (VEt), therefore, consists of the effectiveness against transmission (VEi), and the infectiousness against susceptibility (VEs).
Since the Delta variant seems to spread from the unvaccinated and a subset of the vaccinated (the breakthrough cases), the argument for vaccine effectiveness may still include infectiousness –though to a lesser degree than previously thought – but should focus more squarely on its effectiveness against susceptibility, or severe outcomes. As reported, the effectiveness of the Pfizer two-dose vaccine against severe outcomes to the Delta variant was estimated to be more than 90% in Canada, the U.K., and in Israel.[15]
Most recent data on vaccine effectiveness
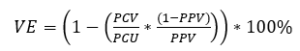
We described the screening method for determining vaccine effectiveness against susceptibility as defined by:
Where:
PCV is the proportion of vaccinated amongst total COVID infections.
PCU is the proportion of unvaccinated amongst total COVID infections (1- PCV).
PPV is the proportion of the population vaccinated.
If we know these values, we can check for ourselves the vaccine effectiveness. We do need to make a choice to decide whether to include partially vaccinated individuals as members of PCV or PCU, and when doing so, adjust the PPV number to be consistent with the choice accepting or rejecting the partially vaccinated.
There is also the question of using data only from the 12+ age category or to use the entire population. We use the entire population data, which is likely marginally optimistic to vaccine effectiveness estimates.
Data taken from the governments of Ontario and Alberta, Canada, from August 10, 2021, to September 18, 2021, were used to make estimates of the vaccine effectiveness against cases, which is an optimistic proxy for transmission, as well as against more severe outcomes such as hospitalization and ICU (intensive-care unit) admissions. [17] [18]A one-month summary of those estimates are given below.
Two findings are evident:
- The effectiveness against cases is estimated at between 79% and 87%.
- The effectiveness against severe outcomes for fully vaccinated individuals is 95%.
Alberta’s relatively low effectiveness of 80% against non-ICU hospitalization warrants further investigation.
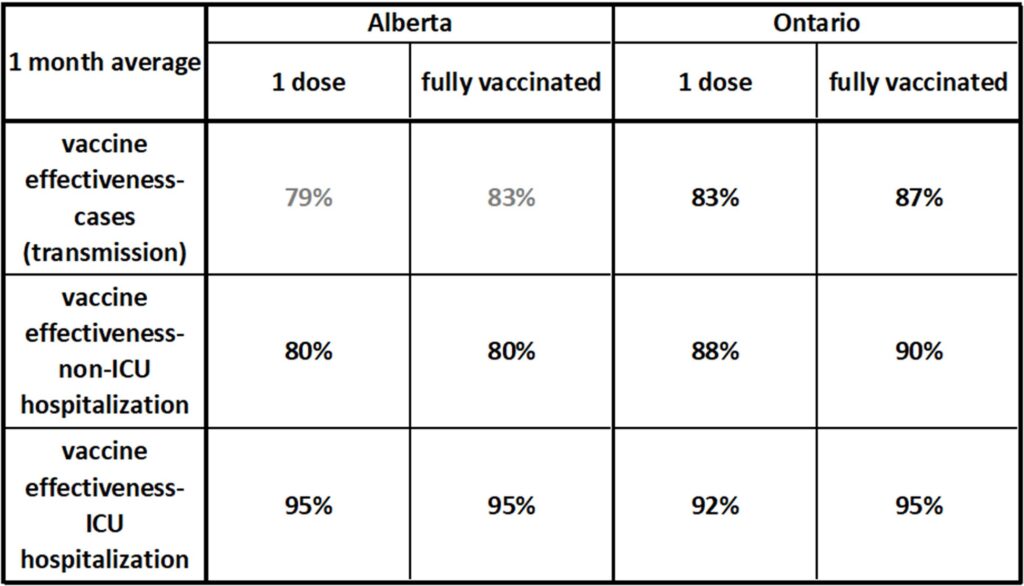
Table showing the vaccine effectiveness (VE) as measured against cases, non-ICU hospitalization, and ICU hospitalization in Ontario and Alberta. The estimates are averaged over the past month. Effectiveness against ICU-level outcomes is estimated at 95%. Data from [19] [20].
The daily data is graphed to see if there is a trend with time. A discernible trend is not clear, except for Alberta’s non-ICU hospitalization curve, which drops over this period.
A key takeaway from this data is that if strained ICU capacity is the bottleneck in society’s functioning through COVID, then vaccination appears to be a highly effective response.
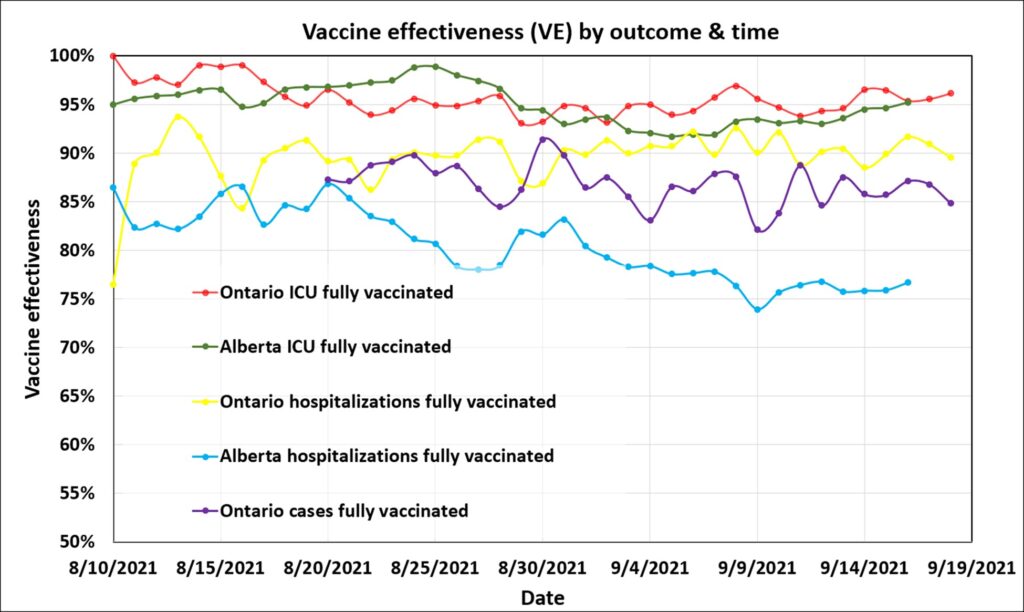
Graph illustrating estimated vaccine effectiveness in Ontario and Alberta, Canada since Aug. 10, 2021. Effectiveness against severe (ICU) outcomes was very high in both provinces at about 95% for fully vaccinated individuals. Alberta’s vaccine effectiveness against non-ICU hospitalization was anomalously low. Data from[21] [22].
Unintended biases
There are at least two unintended biases in the method.
First, the screening method used here depends on the data-collection process. For case data, which is most indicative of transmission and the mildest susceptibility, vaccine effectiveness will likely be optimistic. This is because individuals who are either asymptomatic or who exhibit very mild symptoms may not present themselves for testing. We simply do not count them because they do not show up to be counted. Given the vaccine’s effectiveness against susceptibility, it can be rationally argued that a higher proportion of vaccinated persons may be asymptomatic spreaders. Thus, there is the potential that using reported case numbers could result in a bias toward higher estimated vaccine effectiveness. The degree of this bias is unknown, but Ontario’s 87% vaccine effectiveness for cases is likely high.
The second unintended bias pertains to the vaccine effectiveness against hospitalization, both non-ICU and ICU. Hospitalization data is more accurate than the case data, as individuals experiencing ICU level symptoms are highly unlikely to avoid presenting themselves for care. So the same optimism bias found in the case data is not a factor. The bias in the hospitalization data resides in the percentage population vaccinated number and the way in which the hospitalization numbers are used. The average length of a hospital visit for a person suffering with COVID is 15 days.[23]This means that the numbers used persist for this period, on average. Since vaccination rates have been rising, the method uses too high of a percentage population vaccinated number for most of the dates. The effect of this is to create a small positive bias to the estimated vaccine effectiveness. The bias amounts to an additional value of vaccine effectiveness between zero and one per cent through this data period, and is ignored as immaterial.
Updated herd immunity chart
Our herd immunity chart, first introduced in this article Predicting vaccination rates and outcomes for the Delta variant, considering vaccine effectiveness is displayed below.[24]It has been updated to include vaccination levels from the U.S. and Canada as coloured circles. [25We plot the coloured circles along the 85% vaccine effectiveness curve, based on our case data. This may be optimistic, but is our best current estimate. It is unlikely, though just possible, to read from this chart that we will reach herd immunity. However, the higher the vaccination rate, the lower the exponential spread of the disease and the lower the strain on ICU hospitalizations.
This chart reinforces the prediction that COVID is likely to be present in North America for an extended period of time. Likely for years, to some degree.
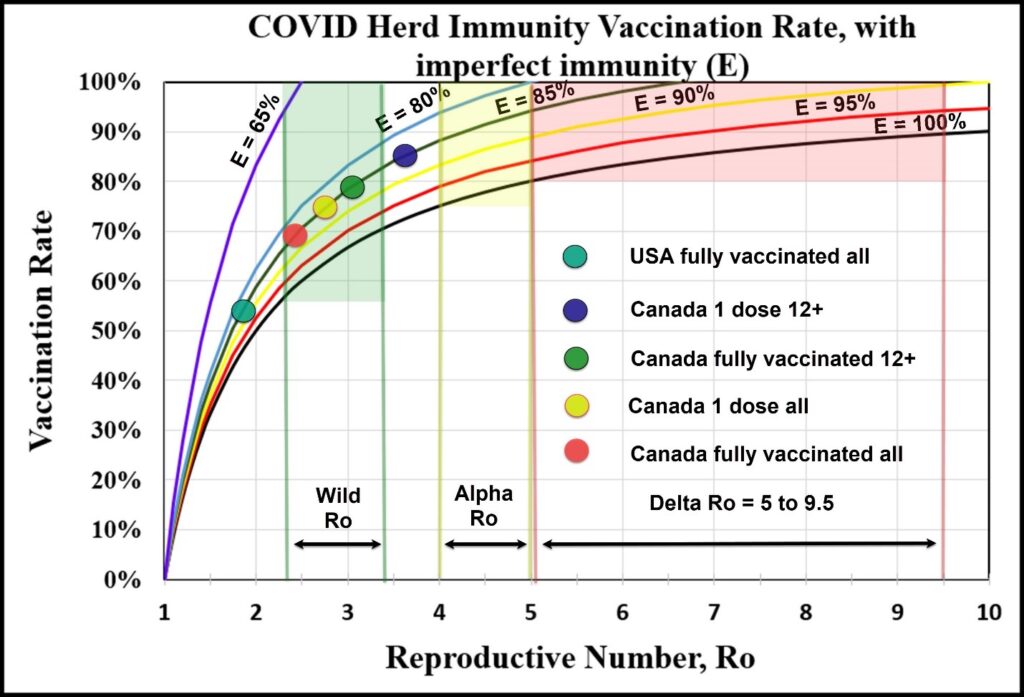
Chart showing the herd immunity vaccination rate prediction for various strains of COVID, accounting for imperfect immunity to transmission. Each line represents the calculation of the herd immunity vaccination rate using a different value for E, or the vaccine effectiveness against transmission. E = 100% coincides with the old curve that was used when the herd immunity rate assumed perfect vaccination effectiveness to transmission. When the curves intersect the 100% “vaccination rate” line on the y-axis, the scenario is considered impossible to eliminate or eradicate the strain. The latest case data out of Canada indicates that E is likely 85% or less. This makes the achievement of herd immunity unlikely. Given certain unintended biases in case reporting (such as individuals not reporting asymptomatic cases), E could be much lower for transmission. Current vaccination levels in the U.S. and Canada are indicated as coloured circles on the chart.[26]
The rational argument for vaccination has changed
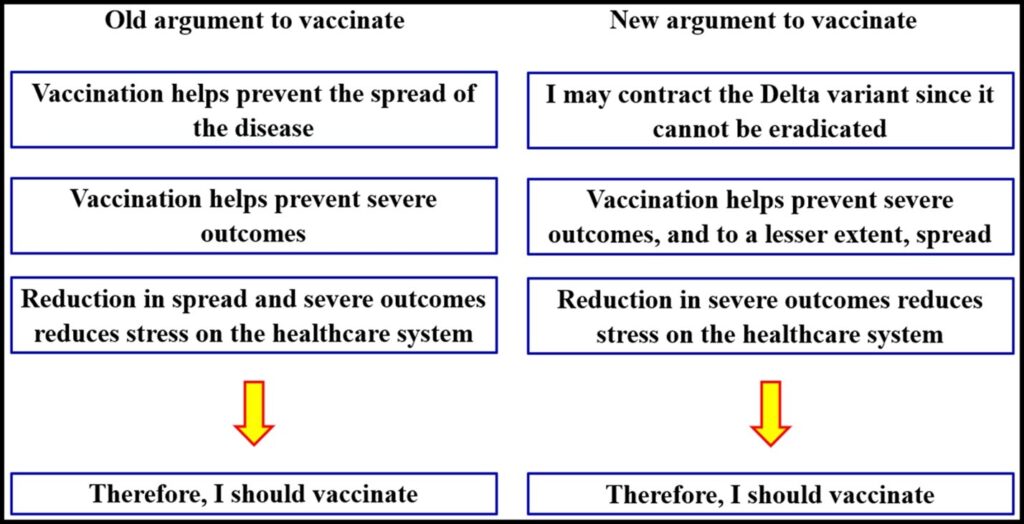
The game-theory argument to vaccinate (or not) uses a particular language, but we can rewrite the problem in terms of critical thinking. This argument has changed with new information. Prior to the evidence of the Delta variant’s transmissibility from even the vaccinated, the principal argument to vaccinate against COVID was:
- Vaccinating helps prevent spread of the disease.
- Vaccinating helps prevent severe outcomes of the disease.
- Reducing spread and severe outcomes reduces stress on the healthcare system.
- Therefore, I should vaccinate.
Given the new information, the principal argument becomes:
- I may eventually contract the Delta variant since it is unlikely to be eradicated.
- Vaccinating helps prevent severe outcomes of the disease. Vaccinating may to a lesser degree reduce spread, though breakthrough cases occur.
- Reducing severe outcomes reduces stress on the healthcare system.
- Therefore, I should vaccinate.
This argument has been summarized below and is an inductive argument, dependent on probabilities.[27]Whether the argument has been strengthened or weakened by this new information regarding the Delta variant is arguable, but it is important that the argument at least be made clearly. Perceptions of vaccine effectiveness and the relative risk of vaccination versus infection are fundamental to the argument.
How does this help us to be calm and manage?
Accepting the situation for what it is will be our first step in a rational response.
We may have predicted that the Delta variant would make eradication of COVID unlikely, but now we are more certain, at least in the near term. Taking the disease’s persistence as highly likely, we can indeed make a rational and calm plan. The argument is this:
- COVID will be with us for some time, perhaps to some extent for several years.
- Vaccines are most effective at preventing severe outcomes. We should vaccinate as much as we can ethically and safely. This will lower hospitalization.
- Given these two premises, we should choose sustainable behaviours – behaviours that we can live with over a period of time of a year or more – to continue functioning as a healthy and productive society.
The point here is not to introduce inflexible policy, but to consider our policy for a period of longer than a few months. Policy must be sustainable from the perspective of mental health and happiness, managing ICU capacity, freedom, and economic productivity. Accepting this need should bring calm, and may help us to chart a more productive path through restrictions, productivity, health, and individuals’ decision to vaccinate.
[1] Coronavirus (COVID-19) Vaccinations, Our World in Data, Sept 3, 2021
[2] Bains, Camille, September 3, 2021, Doctors frustrated with ‘selfishness’ of anti-vaccine protestors, people unvaccinated against COVID-19, The Globe and Mail
[3] Khullar, Dhruv, July 16, 2021, Treating the Unvaccinated, The New Yorker
[4] Hunt, Lee, August 30, 2021, Prisoner’s Dilemma and vaccination, BIG Media
[5] Short, Dylan, Sept 3, 2021, Kenny decries ‘crisis of the vaccinated’ while announcing $100 incentives, Calgary Herald
[6] Hunt, Lee, August 3, 2021, Understanding vaccine effectiveness and breakthrough, BIG Media
[7] Hunt, Lee, August 16, 2021, Predicting vaccination rates and outcomes for the Delta variant, BIG Media
[8] Bains, Camille, September 3, 2021, Doctors frustrated with ‘selfishness’ of anti-vaccine protestors, people unvaccinated against COVID-19, The Globe and Mail
[9] Hunt, Lee, August 30, 2021, Prisoner’s Dilemma and vaccination, BIG Media
[10] Galvani, Alison, Timothy Reluga, Gretchen Chapman, 2007, Long-standing influenza vaccination policy is in accord with individual self interest but not with the utilitarian optimum, PNAS, Vol.104, No. 13, 5692-5697
[11] Bauch, Chris, David Earn, 2004, Vaccination and the theory of games, PNAS, Vol.101, No. 36, 13391-13394
[12] Hunt, Lee, August 3, 2021, Understanding vaccine effectiveness and breakthrough, BIG Media
[13] Halloran, Elizabeth, Ira Longini, and Claudio Struchiner, 1999, Design and Interpretation of Vaccine Field Studies, Epidemiological Reviews, Vol 21, No. 1, 73-88
[14] Halloran, Elizabeth, Ira Longini, and Claudio Struchiner, 1999, Design and Interpretation of Vaccine Field Studies, Epidemiological Reviews, Vol 21, No. 1, 73-88
[15] Hunt, Lee, August 3, 2021, Understanding vaccine effectiveness and breakthrough, BIG Media
[16] Hunt, Lee, August 3, 2021, Understanding vaccine effectiveness and breakthrough, BIG Media
[17] Alberta Health Services, COVID-19 Alberta statistics
[18] Ontario Government, Sept 19, 2021, COVID-19 vaccinations data
[19] Alberta Health Services, COVID-19 Alberta statistics
[20] Ontario Government, Sept 19, 2021, COVID-19 vaccinations data
[21] Alberta Health Services, COVID-19 Alberta statistics
[22] Ontario Government, Sept 19, 2021, COVID-19 vaccinations data
[23] Canadian Institute for Health Information, COVID-19 hospitalization and emergency department statistics
[24] Hunt, Lee, August 16, 2021, Predicting vaccination rates and outcomes for the Delta variant, BIG Media
[25] Coronavirus (COVID-19) Vaccinations, Our World in Data, Sept 3, 2021
[26] Coronavirus (COVID-19) Vaccinations, Our World in Data, Sept 3, 2021
[27] Canadian Institute for Health Information, COVID-19 hospitalization and emergency department statistics
(Lee Hunt – BIG Media Ltd., 2021)